Emergency Medicine 13
Session: Emergency Medicine 13
554 - From Reduction to Release: Optimizing Sedation to Discharge Time for Pediatric Orthopedic Patients in the PED
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 554.4634
Jessica Hayes, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Barron Frazier, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; David Ebenezer, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Jillian Wolf, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Tucker Anderson, Monroe Carell Jr. Children's Hospital at Vanderbilt, Franklin, TN, United States
.jpg)
Jessica Hayes
Resident Physician
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background: Many children who present to the pediatric emergency department (PED) have fractures that can undergo bedside reduction followed by safe discharge. We appreciated many inefficiencies following sedation, primarily in completing and interpreting post-reduction imaging and identifying discharge-ready patients.
Objective: To decrease time from sedation end to discharge by 50% for all patients undergoing fracture reduction in the PED from May 2023 to May 2025.
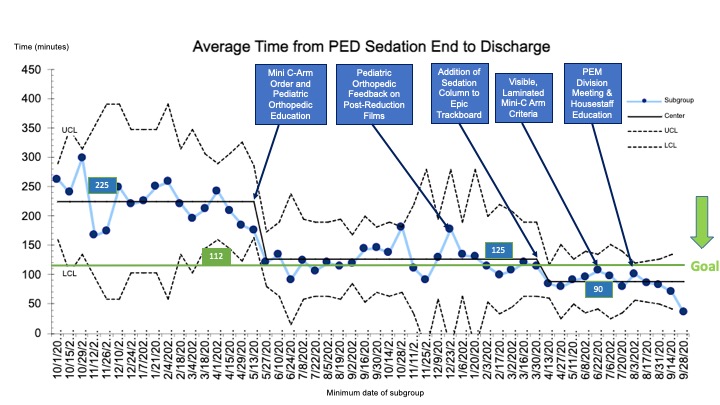
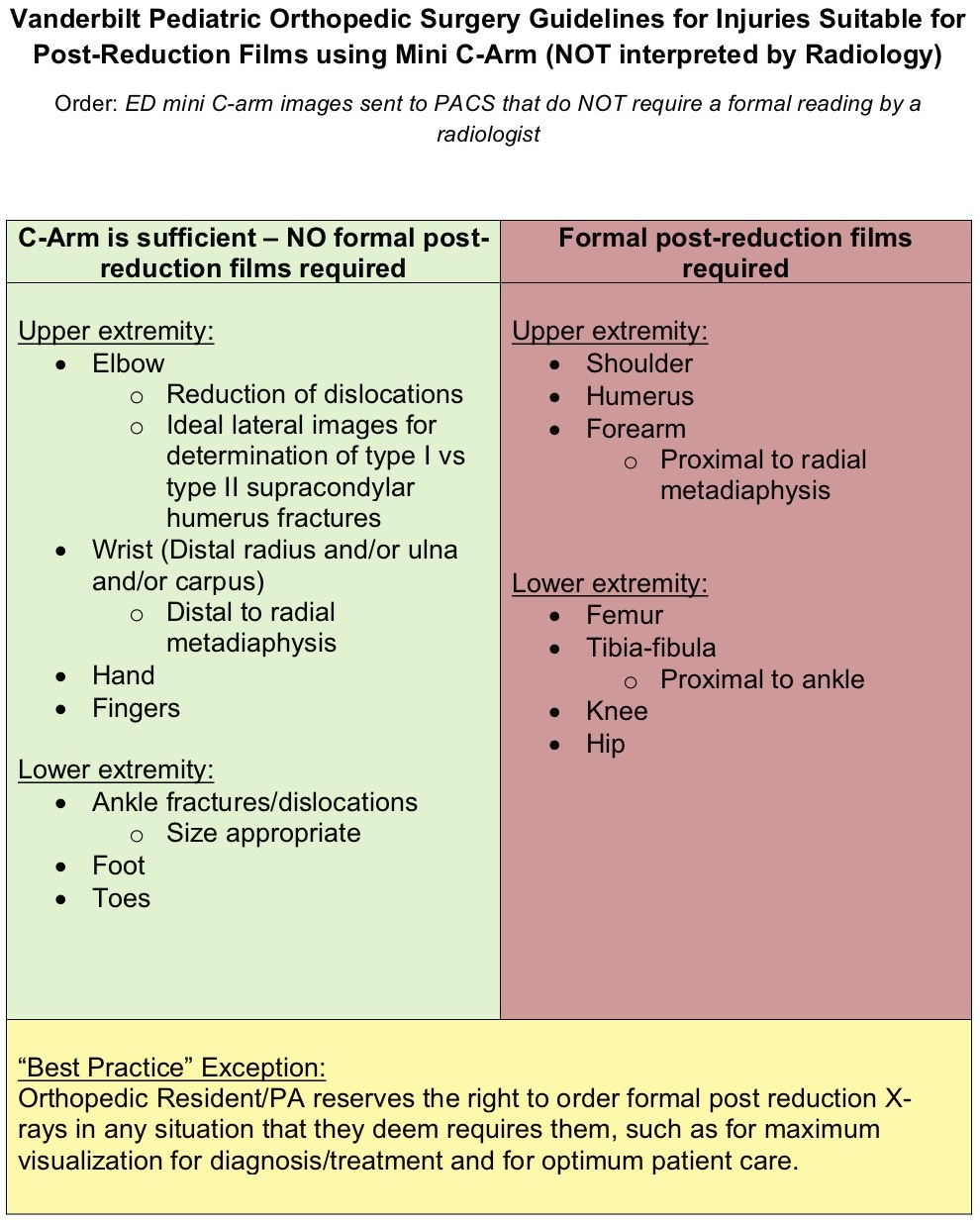
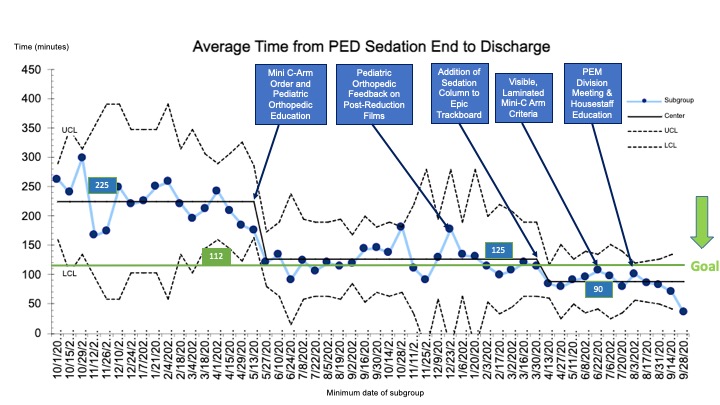
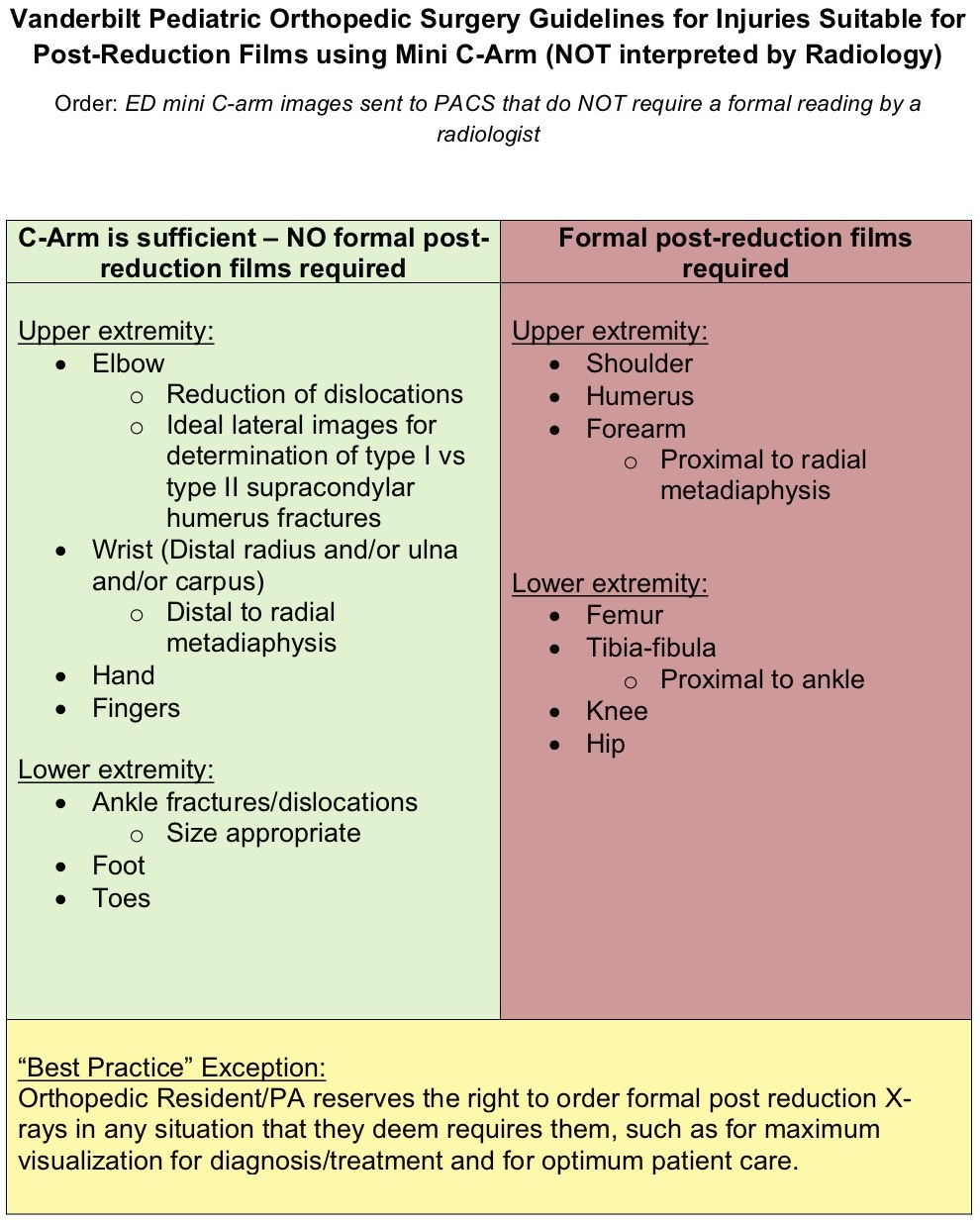
Design/Methods: A multidisciplinary team was formed in 05/2023 and developed a key driver diagram (Figure 1). Retrospective baseline data were obtained from 10/22 through 05/23, after which data were followed prospectively. The population included children ≤ 18 who had a sedated reduction in the PED and met fracture inclusion criteria (Figure 2). Patients were excluded if they met fracture exclusion criteria (Figure 2) or required surgery, admission, or full trauma evaluation.
The primary outcome was average time from sedation end to discharge. Statistical process control charts, including Xbar-S charts and p-charts, were used to analyze data. Process measures included average time from sedation end to discharge for patients with and without post-reduction films and percentage of encounters with post-reduction films. In 05/23, the team implemented a new method to upload images in real-time from the portable x-ray machine (Mini C-arm), obviating the need for post-reduction studies. In 04/24, a sedation column was added to the PED trackboard. Additional interventions included a laminated inclusion criteria sheet attached to the Mini C-arm and ongoing education to residents and faculty.
Results: Of 308 encounters, baseline data represented 68 encounters with an average time from sedation end to discharge of 225 minutes. Following Mini C-arm imaging, special cause variation was detected with a centerline shift to a new sustained average of 125 minutes (Figure 3). With the new sedation column, the average time decreased further to 90 minutes. Formal post-reduction studies appropriately decreased from 100% to 47% of encounters. Patients who had Mini C-arm images only were discharged 36 minutes faster on average than those with post-reduction films.
Conclusion(s): We effectively reduced the time from PED sedation end to discharge by 61% over 17 months. Crucial to these improvements was multidisciplinary involvement to better identify patients who could qualify for Mini C-arm imaging use as a means of reduction success as well as improved unit awareness of patients’ discharge readiness. Ongoing efforts are focused on reducing pre-sedation length of stay.
Key Driver Diagram
.jpg)
Laminated Inclusion and Exclusion Criteria for Exclusive Mini C-Arm Use
Annotated Xbar chart of primary outcome showing average time from PED sedation end to discharge
Key Driver Diagram
.jpg)
Laminated Inclusion and Exclusion Criteria for Exclusive Mini C-Arm Use
Annotated Xbar chart of primary outcome showing average time from PED sedation end to discharge