Children with Chronic Conditions 4
Session: Children with Chronic Conditions 4
470 - “It’s my life and not theirs.” Health and Medical Decision Preferences in Adolescents and Young Adults with Congenital Heart Disease
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 470.3658
Rebecca Delaney, University of Utah, Salt Lake City, UT, United States; Ritika Nayan, University of Utah School of Medicine, Lehi, UT, United States; Katherine C. Boyce, University of Utah School of Medicine, Salt Lake City, UT, United States; Tiffany (Thu) N. Nguyen, University of Utah School of Medicine, West Haven, UT, United States; Ian Lindsay, University of Utah School of Medicine, Salt Lake City, UT, United States; Erin Rothwell, University of Utah, Salt Lake City, UT, United States; Nelangi Pinto, Seattle Children's, Seattle, WA, United States; Angie Fagerlin, University of Utah, Salt Lake City, UT, United States

Rebecca Delaney, PhD (she/her/hers)
Assistant Professor
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Adolescents and young adults (AYAs) with chronic diseases, like congenital heart disease (CHD), should actively engage in their care and decision-making to maintain their health into adulthood. While active or shared decision-making is often recommended for pediatric patients managing chronic diseases, the roles and preferences of pediatric CHD patients are less understood. As this population grows, it is crucial to understand the decisions adolescents and young adults face and their actual and preferred roles in these decisions.
Objective: To understand AYAs’ roles and health-related decision-making preferences in the context of congenital heart disease care.
Design/Methods: AYAs with congenital heart disease, aged 15-21 years, were recruited for virtual semi-structured interviews. During the interviews, participants described a recent medical or health-related decision they made and completed two pie charts: one represented the perceived role of individuals involved and a second showed their desired levels of individuals involved. Additional questions addressed factors influencing their decisions, barriers and facilitators, and preferences for involvement as they age. All interviews were audio recorded, transcribed, and thematically analyzed.
Results: Twenty participants, including 10 adolescents ( < 18 yo) and 10 young adults (≥18 yo), completed interviews. The median age was 17.5 years, with 55% female, 70% Non-Hispanic White, 25% Hispanic, and 5% biracial. Health-related decisions included surgical procedures, physical activity, care management, and disease management (e.g., medication). All but one participant indicated some involvement in the decision, with varying degrees of participation (e.g., Figure 1). Barriers to engagement included lack of knowledge, feeling undervalued, and deferring the decision to parents due to being “too young.” Most participants either desired a more active role (47%) or felt they had sufficient involvement (41%). Parents and clinicians also had prominent roles in the decisions—where both provided information and advice (e.g., pros and cons) and knowledge that informed the decision. Some parents also took a more supportive role in the decision-making process (e.g., “I felt like I was in control but I was still being supported by my mom”), whereas others described their parents as the “ultimate decision-makers.”
Conclusion(s): While AYAs desire to be involved in healthcare decisions, knowledge barriers need to be addressed to facilitate their involvement. Enhancing support for decision-making among the AYA, parent, and clinician triad is essential to meet AYAs’ needs.
Figure 1
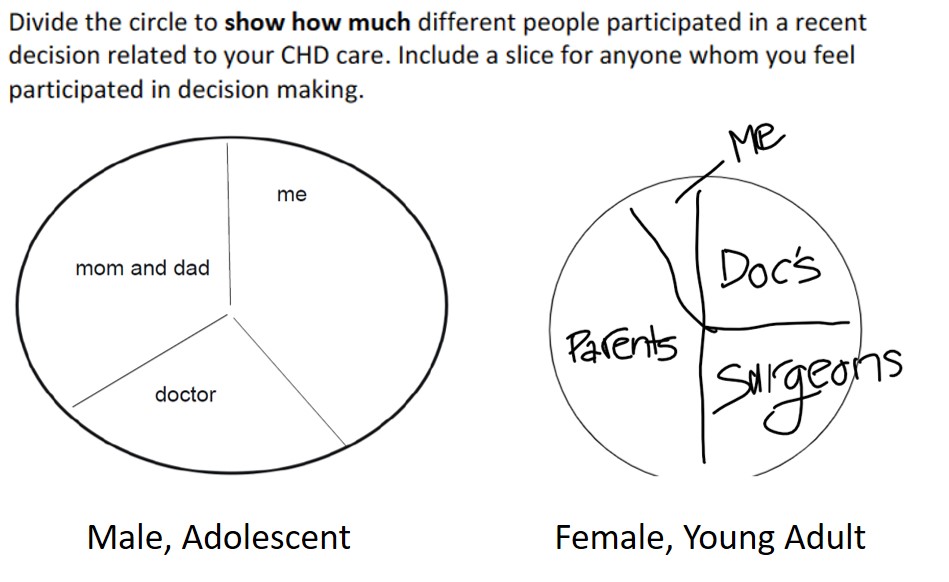 Sample responses from participants on individuals' roles in decisions.
Sample responses from participants on individuals' roles in decisions.
