Emergency Medicine 14
Session: Emergency Medicine 14
566 - “It’s Kind of a Pickle” – Evaluation of Pediatric Appendicitis and Opportunities for Shared Decision-Making in Community Emergency Departments
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 566.3649
Courtney W.. Mangus, C.S. Mott Children's Hospital, Ann Arbor, MI, United States; Sarah J. Parker, University of Michigan Medical School, Ann Arbor, MI, United States; Anupam B. Kharbanda, Chidlrens Minnesota, Minneapolis, MN, United States; Brian J. Zikmund-Fisher, University of Michigan, Ann Arbor, MI, United States; Melissa Brooks, University of Michigan Medical School, Flint, MI, United States; Helene M.. Epstein, Patients for Patient Safety, Stamford, CT, United States; Emma Griffin, University of Michigan, Grosse Ile, MI, United States; Bryan Judge, Michigan State University College of Human Medicine, Ada, MI, United States; Aparna Joshi, University of Michigan Medical School, Ann Arbor, MI, United States; Heather Orman-Lubell, True North Pediatrics, Flourtown, PA, United States; Milisa Manojlovich, University of Michigan, Ann Arbor, MI, United States; Brigid Rice, Johns Hopkins Howard County Medical Center, Catonsville, MD, United States; Gul R. Sachwani-Daswani, Hurley Medical Center, Flint, MI, United States; Suz Schrandt, ExPPect, Arlington, VA, United States; K. Elizabeth Speck, University of Michigan Health System, Ann Arbor, MI, United States; Prashant Mahajan, University of Michigan Medical School, Troy, MI, United States; Elizabeth Schoenfeld, UMass Chan - Baystate, Department of Emergency Medicine, Department of Healthcare Delivery and Population Science, Springfield, MA, United States

Courtney W. Mangus, MD, MS (she/her/hers)
Assistant Professor
C.S. Mott Children's Hospital
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Pediatric abdominal pain accounts for over one million emergency department (ED) visits annually. Appendicitis, the most common surgical diagnosis, is typically confirmed by imaging. Current guidelines recommend ultrasound as the initial study. However, due to variable availability and expertise in interpretation of ultrasound in community EDs, clinicians in this setting often obtain computed tomography (CT) for diagnosis. Although CT has optimal diagnostic performance, it involves exposure to ionizing radiation which increases the risk of malignancy. Shared decision-making (SDM) between ED providers and families is a unique approach to optimize evaluation options and avoid unnecessary CTs. Currently, there is no guidance on when and how to pursue SDM in community ED evaluation of pediatric abdominal pain concerning for appendicitis.
Objective: To understand current diagnostic approaches including the use of SDM and existing decision-support tools such as the pediatric Appendicitis Risk Calculator (pARC) and develop a conceptual model for SDM in the community ED evaluation of suspected pediatric appendicitis.
Design/Methods: A steering group of relevant experts developed an interview guide based on the objectives. Using a qualitative study design, we conducted semi-structured interviews with 15 community ED physicians. Interviews were analyzed using a hybrid thematic approach.
Results: We identified six themes (Table 1) related to the diagnostic process and role of SDM:
1) The limited availability and diagnostic utility of ultrasound often precludes routine use; 2) Clinicians tend to rely on gestalt over clinical scoring tools or practice guidelines; 3) SDM is employed frequently but at variable points in the diagnostic process; 4) The pARC tool could be improved with integration of community-specific recommendations for patients at intermediate risk; 5) Guidelines regarding transfer of patients to pediatric centers prior to definitive imaging are needed; 6) Clinicians desire a standardized tool to guide their diagnostic evaluation and SDM discussions regarding risk of appendicitis and radiation exposure. Interview data informed the creation a conceptual model to illustrate the potential role of pARC and SDM in the diagnostic process (Figure 1).
Conclusion(s): The evaluation of pediatric abdominal pain in community EDs often involves SDM at multiple stages. Adapting a validated clinical decision-support tool (such as pARC) to include community ED-specific guidelines could enhance SDM, optimize diagnostic safety, and reduce patient harm from unnecessary radiation.
Table 1. Key themes and corresponding quotes from community ED physicians
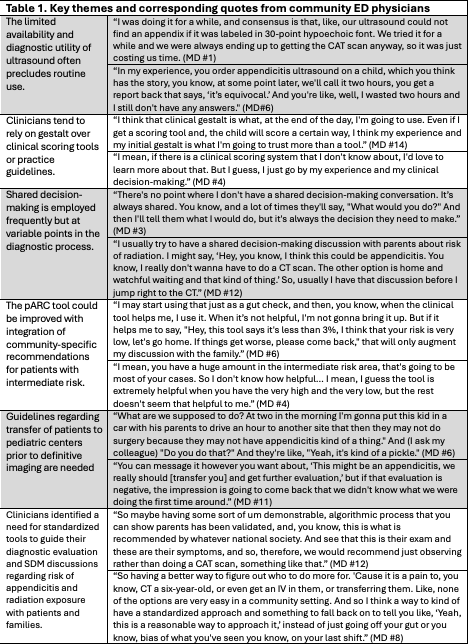
Figure 1. Opportunities for shared decision-making (SDM) in the diagnostic evaluation of a child with possible appendicitis who presents to a community emergency department.
.png) Potential opportunities for SDM are shown in purple boxes.
Potential opportunities for SDM are shown in purple boxes. Table 1. Key themes and corresponding quotes from community ED physicians
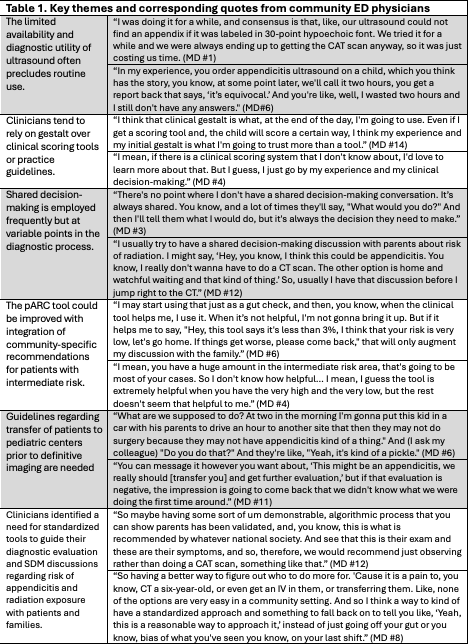
Figure 1. Opportunities for shared decision-making (SDM) in the diagnostic evaluation of a child with possible appendicitis who presents to a community emergency department.
.png) Potential opportunities for SDM are shown in purple boxes.
Potential opportunities for SDM are shown in purple boxes. 
