Health Equity/Social Determinants of Health 11
Session: Health Equity/Social Determinants of Health 11
212 - Association of Social Risk Factors and Insurance Provider Status with Metabolic Syndrome Diagnosis at Baseline in Youth Referred for Hypertension Disorders: An Analysis of the SUPERHERO Data
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 212.3861
Elizabeth A. Onugha, Baylor College of Medicine, Houston, TX, United States; Sahar Siddiqui, Texas Children's Hospital, Houston, TX, United States; Jessica Fallon. Campbell, Baylor College of Medicine, Houston, TX, United States; Ashna Pudupakkam, Baylor College of Medicine, Houston, TX, United States; Landon T. Sanz, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Spring, TX, United States; Sandeep Riar, Children's Healthcare of Atlanta, Atlanta, GA, United States; Margaret Murphy, University of Kentucky College of Medicine, Lexington, KY, United States; Andrew M. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States

Elizabeth A. Onugha, MD MSCI (she/her/hers)
Assistant Professor
Baylor College of Medicine
The Woodlands, Texas, United States
Presenting Author(s)
Background: Metabolic syndrome (MetS) disproportionately affects low-income individuals and is associated with cardiovascular mortality. The association of social disadvantage and insurance coverage with MetS has been studied in adults. The data in children is sparse.
Objective: We set out to assess the association between social risk factors, insurance status and MetS in youth with hypertension (HTN) disorders.
Design/Methods: We conducted a cross-sectional analysis of baseline data from the Study of the Epidemiology of Pediatric Hypertension (SUPERHERO), a retrospective Registry of electronic health record data obtained using standardized and validated biomedical informatics scripts. Inclusion criteria were youth < 19 years old who received care from subspecialists for HTN disorders from 1/1/2016–12/31/2023 defined by ICD-10 codes. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 codes. The outcome was MetS defined by ICD-10 codes. Exposures were the presence of at least one social risk factor defined by ICD-10 codes and included food access, transportation, housing, income, education, employment, family, and crime and insurance provider status categorized as government sponsored insurance, private insurance and self-pay. We used unadjusted generalized linear models to evaluate this association.
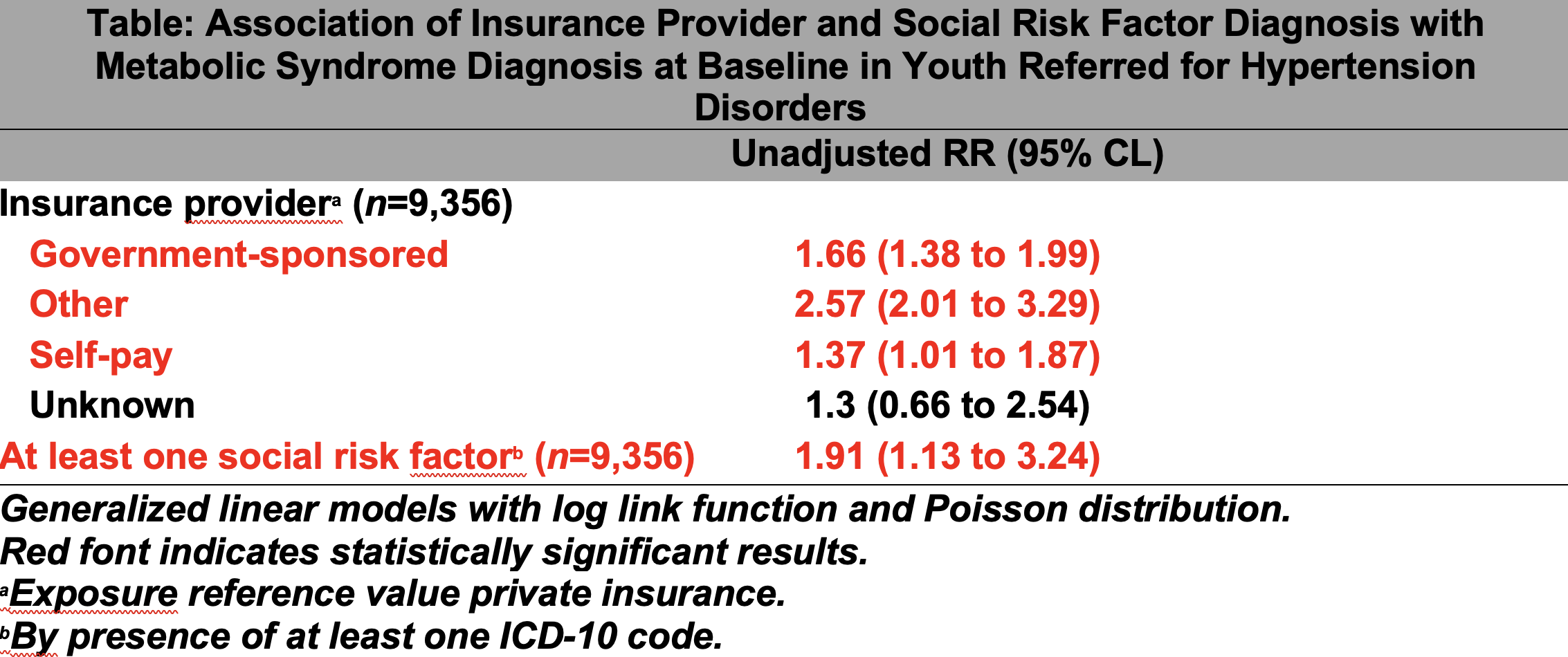
Results: Of 9,356 participants, the median age was 14.0 years (IQR 10.5, 16.3) and 3,544 (38%) were female. The prevalence of MetS was 10%. 74 (0.8%) youth had at least one social risk factor. 2,147 (23%) had private insurance while 5,736 (61%) had government-sponsored insurance. Participants with at least one social risk factor were almost twice as likely to have MetS (RR 1.91, 95% CL 1.13 to 3.24). Participants with government insurance were 1.66 times more likely (RR 1.66, 95 CL 1.38- 1.99) to have metabolic syndrome.
Conclusion(s): Among youth referred for HTN disorders, we found that those with at least one social risk factor and those with government insurance were more likely to have MetS. Given the low prevalence of social risk factors by ICD-10 codes in this early SUPERHERO phase, there is a critical need for a multidisciplinary approach to more comprehensively screen for and identify social risk factors in this at-risk population. Identifying and addressing social needs in patients with MetS is a priority that will allow health personnel to efficiently treat the condition over the life course and mitigate adverse cardiovascular consequences. Future SUPERHERO analysis will investigate the impact of interventions addressing social risk factors on MetS health outcomes.
Association of Insurance Provider Status and Social Risk Factors with Metabolic Syndrome