Emergency Medicine 14
Session: Emergency Medicine 14
570 - Comparative Diagnostic Performance of Masonic vs. Referral Ultrasound in Pediatric Appendicitis Using pARC Scores
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 570.4073
Vitaliy Perepelitsa, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Jeffrey P. Louie, University of Minnesota Medical School, Minneapolis, MN, United States; Jeffrey Ames, University of Minnesota, Mounds View, MN, United States; Kari Schneider, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Rahul Kaila, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Pablo U. Avendano, University of Minnesota Masonic Children’s Hospital, Plymouth, MN, United States

Vitaliy Perepelitsa, DO (he/him/his)
Resident physician
University of Minnesota Masonic Children's Hospital
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Acute appendicitis is the most common cause of acute abdominal pain that requires surgical treatment with more than 75 000 children diagnosed annually in the United States. Our institution repeats appendicitis Ultrasounds on all patients refereed to us for acute appendicitis.
Objective: To compare the diagnostic performance of Pediatric ED versus referral ED ultrasound (US) in detecting acute appendicitis when applying pARC score (Pediatric Appendicitis Risk Calculator).
Design/Methods: This was a secondary analysis from a retrospective database involving four general emergency departments. The study focused on children under 18 years of age evaluated for suspected appendicitis. All children underwent an ultrasound at the referral facility and again upon arrival at the pediatric emergency department. The Pediatric Appendicitis Risk Calculator (pARC) scores from referral ED and Pediatric ED were compared against pathology results and Masonic US overreads. Sensitivity and correlation with pARC scores were assessed for both Masonic and referral US. Fisher's exact test was used to evaluate the statistical significance of differences in diagnostic performance between Masonic and referral US.
Results: Pediatric US demonstrated a higher sensitivity (85.2%) compared to referral US (51.9%) in diagnosing appendicitis. Fisher’s exact test revealed a significant difference between the two modalities (p = 0.018), with an odds ratio of 5.34, indicating that Pediatric US was significantly more likely to correctly diagnose appendicitis than referral US. Additionally, Pediatric US showed a stronger alignment with higher pARC scores (≥50%), enhancing its diagnostic accuracy in identifying true positive cases of appendicitis.
Conclusion(s): Pediatric ED US outperforms referral US in diagnosing acute appendicitis when pARC scores are applied, with a statistically significant improvement in sensitivity and diagnostic consistency. These findings support the use of Pediatric US as the preferred imaging modality for patients with moderate to high pARC scores, optimizing the accuracy of appendicitis diagnosis and guiding clinical management.
Table 1: Demographics and Data
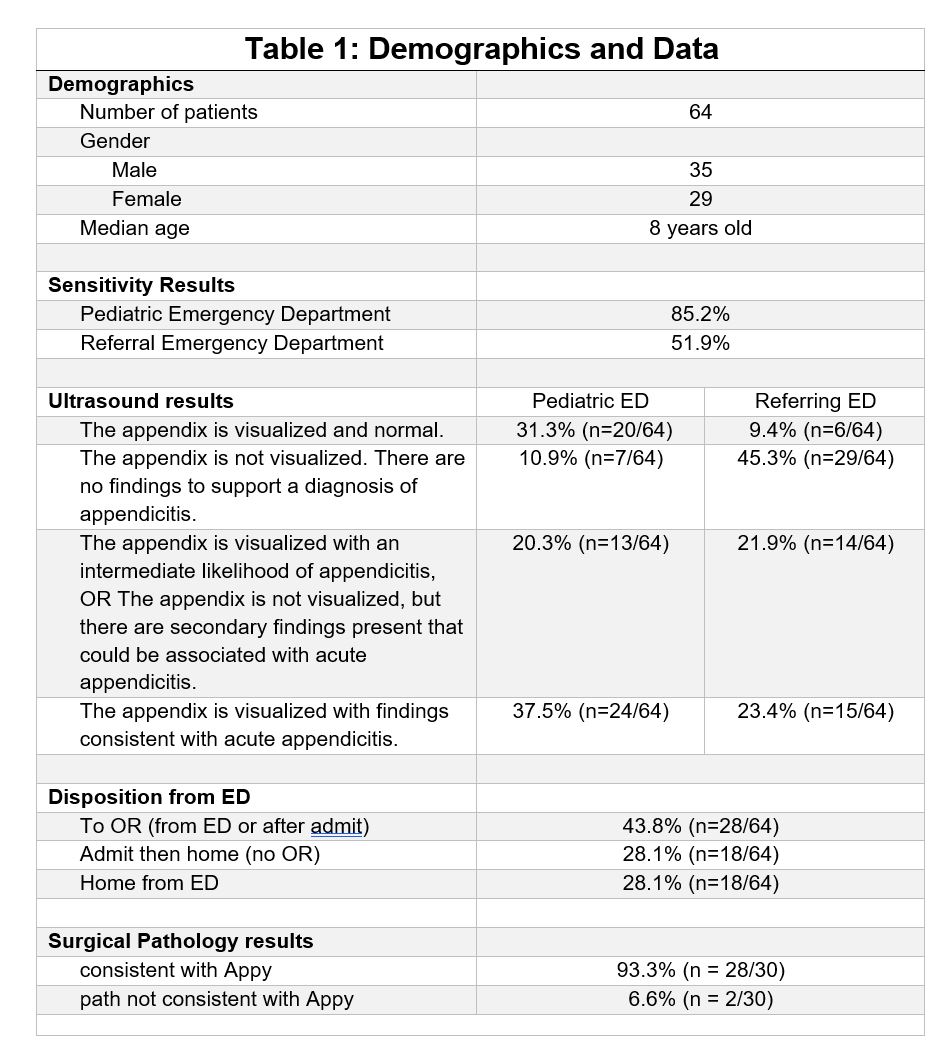 Demographics and Data
Demographics and DataTable 1: Demographics and Data
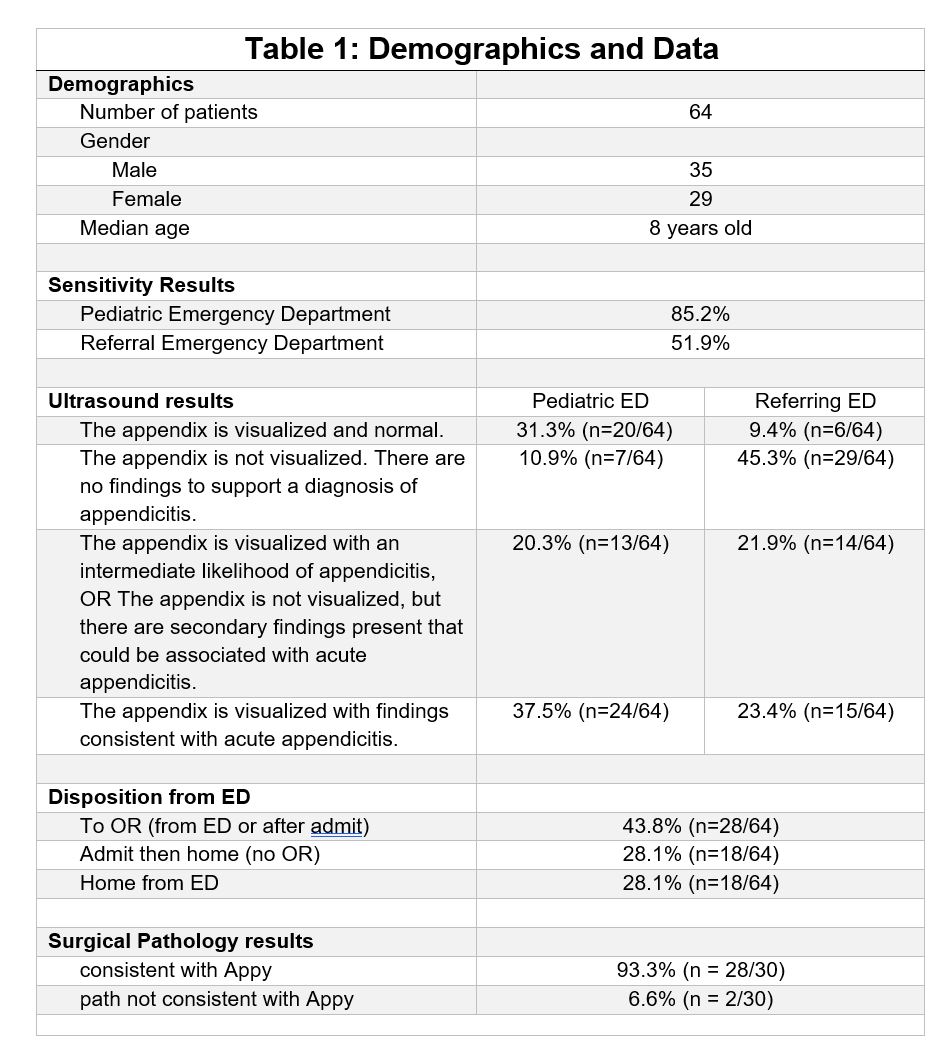 Demographics and Data
Demographics and Data
