Adolescent Medicine 5: Potpourri
Session: Adolescent Medicine 5: Potpourri
135 - Beyond Early Childhood: Adolescent Health Outcomes in Preterm-Born Infants from a Population-Based Cohort Study in British Columbia, Canada
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 135.3923
Sumera Aziz, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; YE SHEN, BC Children's Hospital Research Institute, Richmond, BC, Canada; Jeffrey N.. Bone, BC Children's Hosiptal Research Institute, Vancouver, BC, Canada; sarka Lisonkova, UBC, Vancouver, BC, Canada; Lindsay Richter, University of British Columbia, Vancouver, BC, Canada; Joseph Ting, University of Alberta, Edmonton, AB, Canada
.jpg)
Joseph Yuk Ting, MD, MPH
Associate Professor
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Despite improvements in newborn care, preterm birth is linked to various long-term health outcomes, extending beyond early childhood and into adolescence. Investigating these outcomes provides critical insights into potential interventions to improve the long-term health and well-being of individuals born preterm.
Objective: This study aimed to assess morbidity among adolescents born preterm from 10 to 17 years of age.
Design/Methods: Utilizing the perinatal data and health registries of British Columbia extracted by Population Data BC (PopData BC), we included adolescents born between 2004 and 2012 at gestational ages (GA) of 22 to 44 weeks who survived beyond 10 years of age with follow-up until 2019. The primary outcome was morbidity, measured through diagnoses recorded from both outpatient and inpatient visits. We employed Cox proportional hazards models and reported adjusted hazard ratios (AHR) with 95% confidence intervals (CIs) adjusted for maternal age, previous pregnancies, region of residence, smoking status, hypertension, diabetes, and prior history of low birth weight, stillbirth, or preterm birth.
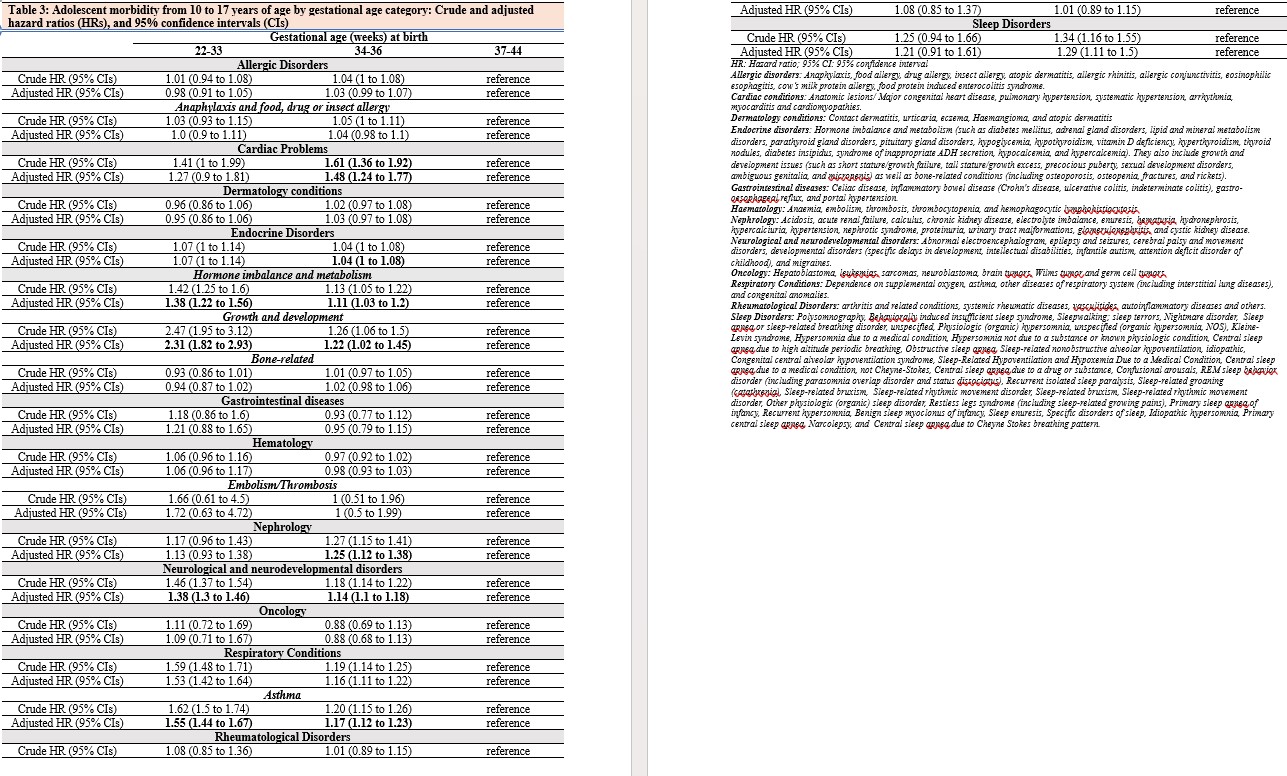
Results: In the cohort of 297,477 adolescents, 2.0% were born at 22-33 weeks GA, 7.2% at 34-36 weeks, and 90.8% at 37-44 weeks GA (Table 1). Across GA categories, preterm infants demonstrated higher rates of adverse health outcomes overall. The risk of respiratory, hormone and metabolic, growth and developmental, endocrine, and neurological and neurodevelopmental disorders increased with decreasing gestational age (Table 2). Compared to adolescents born at 37-44 weeks GA, preterm-born adolescents had significantly elevated risks of cardiac (AHR: 1.27 to 1.48), endocrine (AHR: 1.04 to 1.07), nephrological (AHR: 1.13 to 1.25), neurological and neurodevelopmental (AHR 1.14 to 2.05), respiratory (AHR: 1.16 to 1.55), and sleep (AHR: 1.21 to 1.29) disorders (Table 3).
Conclusion(s): This population-based cohort study underscores the long-term health implications of preterm birth, revealing a significant association between decreased gestational age and increased morbidity during adolescence. These findings underscore the necessity for targeted healthcare interventions and policy development aimed at addressing the specific health challenges encountered by adolescents born preterm, ultimately improving their long-term health trajectories.
CV_Sumera_Aziz.pdf
Number and rates of adolescent health outcomes* by gestational age, n (%)
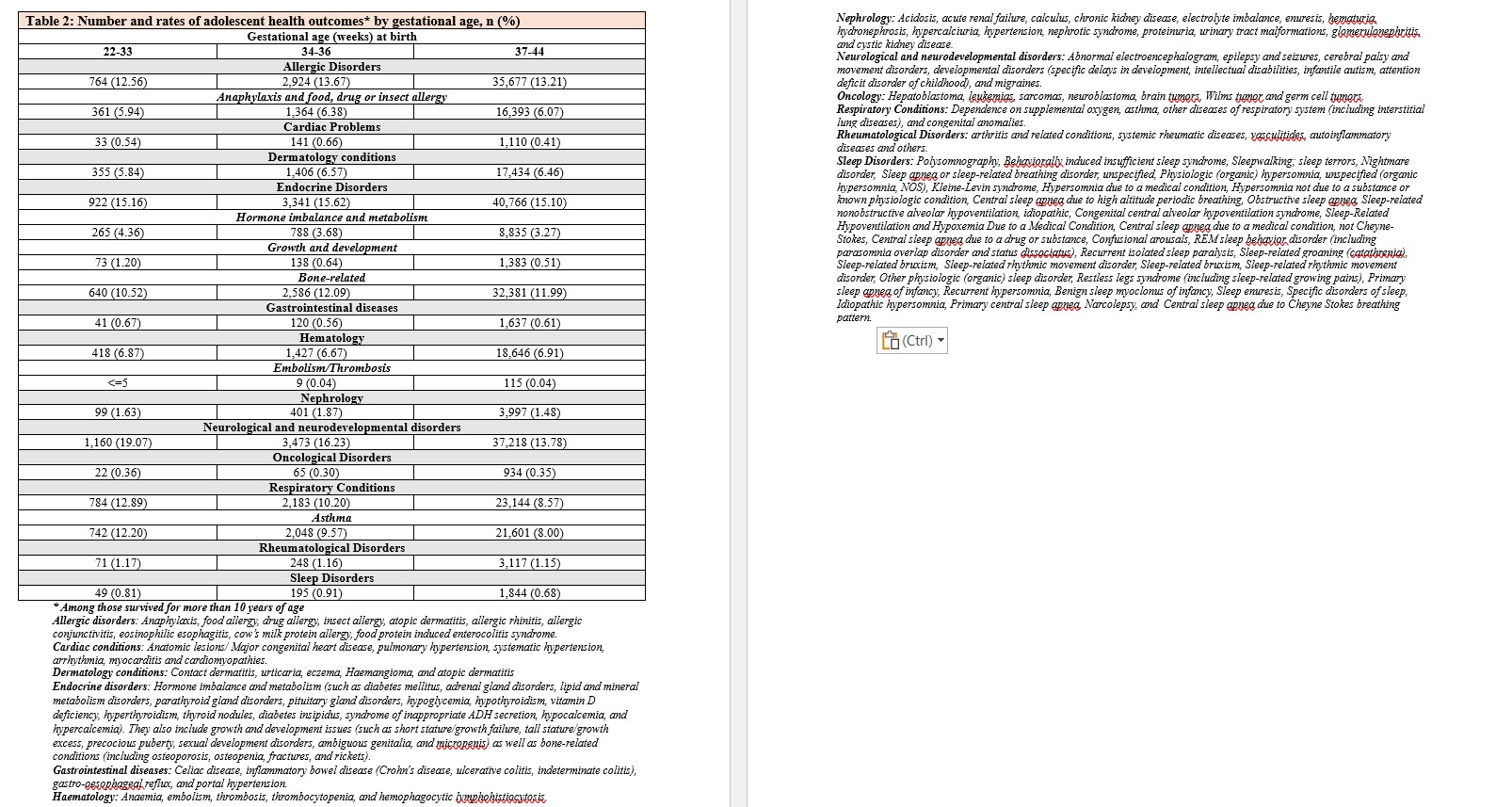
Adolescent morbidity from 10 to 17 years of age by gestational age category: Crude and adjusted hazard ratios (HRs), and 95% confidence intervals (CIs)