Emergency Medicine 10
Session: Emergency Medicine 10
517 - Increasing balanced fluid resuscitation for sepsis patients in a tertiary care pediatric emergency department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 517.5213
Grace E. Arends, Children's Mercy Hospitals and Clinics, Shawnee, KS, United States; Christopher Kaberline, Children's Mercy Hospitals and Clinics, Prairie Village, KS, United States; Sarah K. Nienhaus, Children's Mercy Hospital, Kansas City, MO, United States; Ibad Siddiqi, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States

Grace E. Arends, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Mercy Hospitals and Clinics
Shawnee, Kansas, United States
Presenting Author(s)
Background: National data supports balanced fluid during volume resuscitation in the setting of sepsis as it has been shown to improve morbidity and mortality, particularly preventing acidosis and kidney injury. Despite this recommendation, the Children’s Mercy Emergency Department still has not implemented balanced fluid resuscitation.
Objective: The aim of the project is to increase the percentage of patients with positive sepsis screen treated in the Children’s Mercy Hospital Adele Hall Emergency Department (CMH ED) receiving lactated ringer’s (LR) fluid resuscitation from 4.6% to 15% by June 2024.
Design/Methods: Primary outcome measures were percentage of patients with suspected sepsis in the CMH ED who received at least one LR fluid bolus, as well as percentage of patients who received LR as their first bolus in fluid resuscitation. Primary process measure was sepsis huddle form usage. The primary balancing measure was the number of LR fluid boluses ordered in the ED for any indication. Fishbone diagram was utilized to identify interventions. The first PDSA cycle (June 2023) included education for the division, updating the sepsis care process model, updating the sepsis order set for LR to be the default fluid ordered, and difficult IV access pathway being published. The second PDSA cycle (July 2023) focused on readily stocking LR in the medication room, surveying physicians about LR usage, and adding a note to the huddle form to recommend LR. The third PDSA (Feb 2024) included float pool education and the sepsis care process model including ceftriaxone and LR incompatibility. The fourth PDSA cycle (May 2024) included nurse reeducation on compatibility. The fifth PDSA cycle (July 2024) linked the sepsis order set to the huddle form. An FMEA was completed between the second and third PDSA cycle to focus on safely implementing balanced fluid given LR and ceftriaxone incompatibility, which further guided interventions.
Results: Data shows a center line shift with sepsis patients receiving at least one balanced fluid bolus (Fig 1) and those sepsis patients receiving first bolus as balanced fluid in the CMH ED (Fig 2). Sepsis huddle compliance improved from 45.6% to 51.74% in June 2023. The number of LR boluses ordered for any indication showed a centerline shift from 32.9 to 165.8 in June 2023 (Fig 3).
Conclusion(s): Through multiple interventions, successful implementation of balanced fluid resuscitation was implemented in the CMH ED. Order set changes and care process model updates seemed to be the most influential changes that were made. FMEA proved to be a helpful tool to ensure safe implementation.
Figure 1: Outcome measure 1- Percentage of sepsis patients receiving at least one lactated ringer’s fluid bolus.
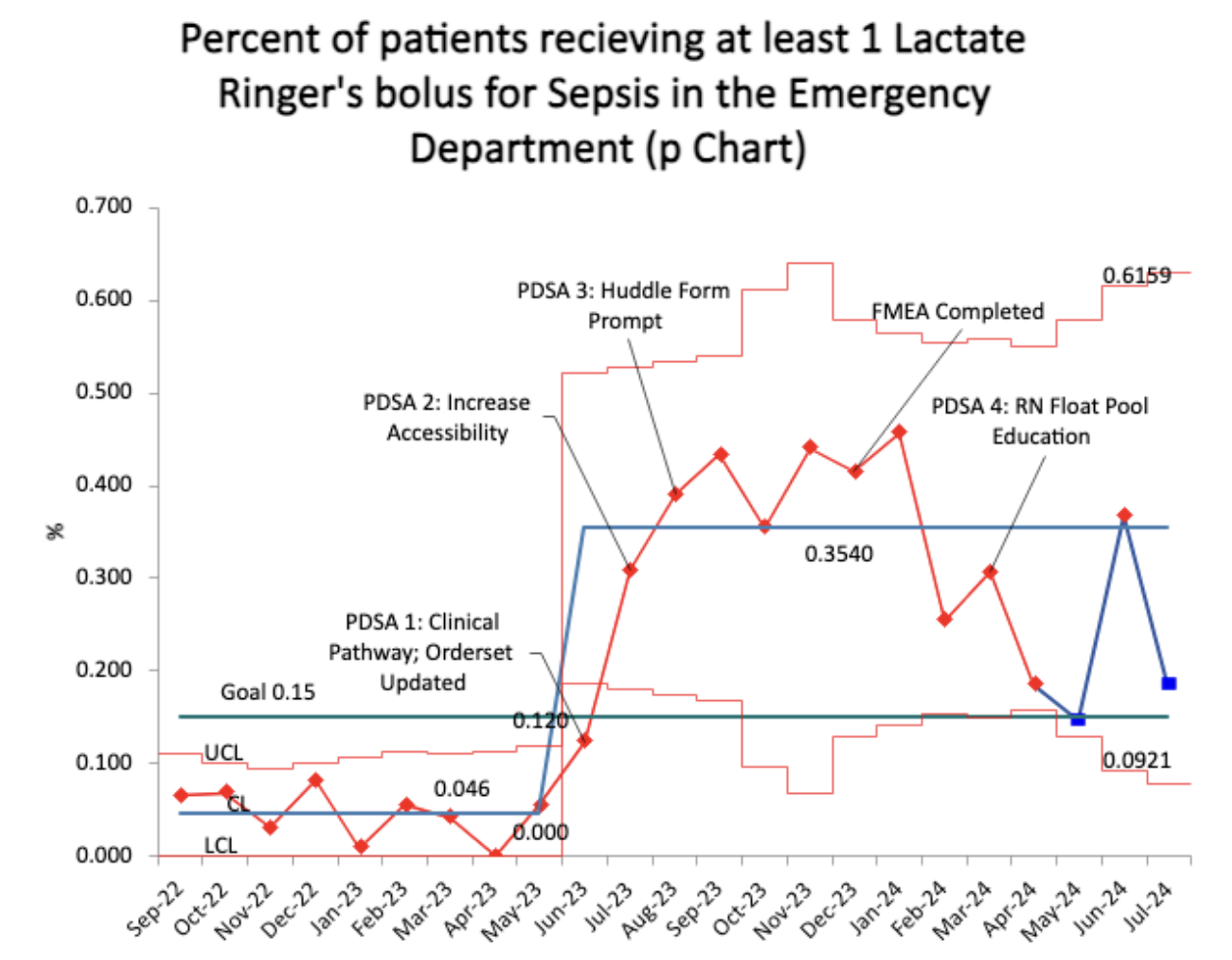 The percentage of lactated ringer’s utilized as any bolus in sepsis fluid resuscitation in the emergency department demonstrated a center line shift in June 2023 from 4.6% to 33.2%
The percentage of lactated ringer’s utilized as any bolus in sepsis fluid resuscitation in the emergency department demonstrated a center line shift in June 2023 from 4.6% to 33.2% Figure 2: Outcome measure 2- Percentage of sepsis patient’s receiving their first fluid bolus as lactated ringer’s.
.png) The percentage of Lactated Ringer’s used as first bolus in the emergency department showed a centerline shift in June 2023 from 4.6% to 33.27%
The percentage of Lactated Ringer’s used as first bolus in the emergency department showed a centerline shift in June 2023 from 4.6% to 33.27% Figure 3: Balance Measure- Number of lactated ringer’s fluid boluses ordered for any other reason.
.png) The number of lactated ringer’s boluses ordered in the CMH Adele Hall ED showed a center line shift in June 2023 from 32.9 a month to 178.6 a month.
The number of lactated ringer’s boluses ordered in the CMH Adele Hall ED showed a center line shift in June 2023 from 32.9 a month to 178.6 a month.

