Neonatal Follow-Up 3: Long-Term Outcomes in NICU Graduates
Session: Neonatal Follow-Up 3: Long-Term Outcomes in NICU Graduates
582 - Evaluating Late Childhood Morbidity: Effects of Maternal BMI and Smoking on Health Outcomes
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 582.5047
Sumera Aziz, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; sarka Lisonkova, UBC, Vancouver, BC, Canada; YE SHEN, BC Children's Hospital Research Institute, Richmond, BC, Canada; Jeffrey N.. Bone, BC Children's Hosiptal Research Institute, Vancouver, BC, Canada; Lindsay Richter, University of British Columbia, Vancouver, BC, Canada; Joseph Ting, University of Alberta, Edmonton, AB, Canada
.jpg)
Joseph Yuk Ting, MD, MPH
Associate Professor
University of Alberta
Edmonton, Alberta, Canada
Presenting Author(s)
Background: Maternal smoking and pre-pregnancy body mass index (BMI) are independently associated with childhood outcomes.
Objective: We assessed whether smoking during pregnancy modified the relationship between pre-pregnancy BMI and late childhood health outcomes.
Design/Methods: A retrospective population-based cohort study of children, with follow up data for 5-10 years, was conducted utilizing data from Population Data BC including the British Columbia Perinatal Data Registry and administrative health databases including the Medical Services Plan (MSP) Payment Information registry, and Discharge Abstract Database. Women were grouped into underweight (BMI < 18.5 kg/m²), normal weight (BMI 18.5–24.9 kg/m²), overweight (BMI 25–29.9 kg/m²), and obese (BMI ≥30 kg/m²). The hypothesized effect modifier was smoking during pregnancy. Outcomes included hospitalizations, emergency (ER) visits, intensive care unit (ICU) admissions, physician consultations, and late childhood morbidity. Poisson regression was used to estimate adjusted risk ratios (ARRs) with 95% confidence intervals (CIs), adjusting for potential confounders, including maternal age, prior pregnancy, region of residence, hypertension, diabetes, prior history of low-birth-weight birth, neonatal death, stillbirth, or preterm birth.
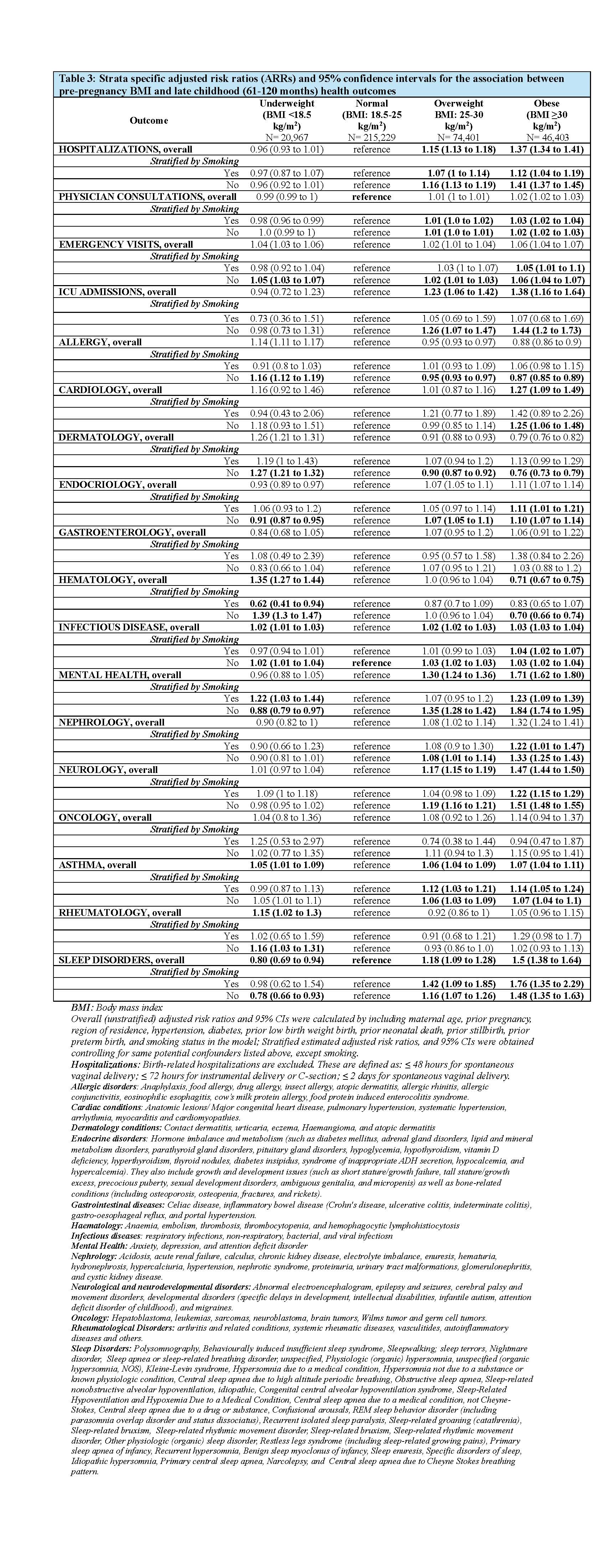
Results: Among 357,000 mothers, 5.8% were underweight, 60% had normal BMI (reference), 20.8% were overweight, and 13% were obese. The prevalence of smoking was 8.09% (Table 1). Compared with children of normal-BMI women, the risk of hospitalizations, physician consultation, ICU admissions, asthma, infections, endocrinology, nephrology, neurology, mental health, and sleep disorders increased with higher maternal BMI. We observed a U-shaped relationship between pre-pregnancy BMI and ER visits. Offspring of underweight vs. normal-BMI women were at increased risk of allergies (ARR: 1.14; 95% CI: 1.10, 1.17), hematology (ARR: 1.35; 95% CI: 1.27, 1.44), dermatology (ARR: 1.26; 95% CI: 1.21, 1.32), and rheumatology (ARR: 1.16; 95% CI: 1.03, 1.31) disorders, whereas obesity was associated with cardiac disorders (ARR: 1.27; 95% CI: 1.09, 1.49). Among smokers, underweight vs. normal-BMI women, children had higher risk of mental health disorders (ARR: 1.22; 95% CI: 1.03, 1.44), with corresponding ARR of 0.88 (95% CI: 0.79, 0.97) among children of non-smokers.
Conclusion(s): Children of overweight or obese mothers may require greater healthcare attention than those of mothers with normal BMI. Smoking modified the effect of pre-pregnancy BMI on certain individual morbidities.
CV_Sumera_Aziz.pdf
Late childhood (61-120 months) outcome rates among women with singleton births by pre-pregnancy BMI, stratified by smoking during pregnancy, n (%)
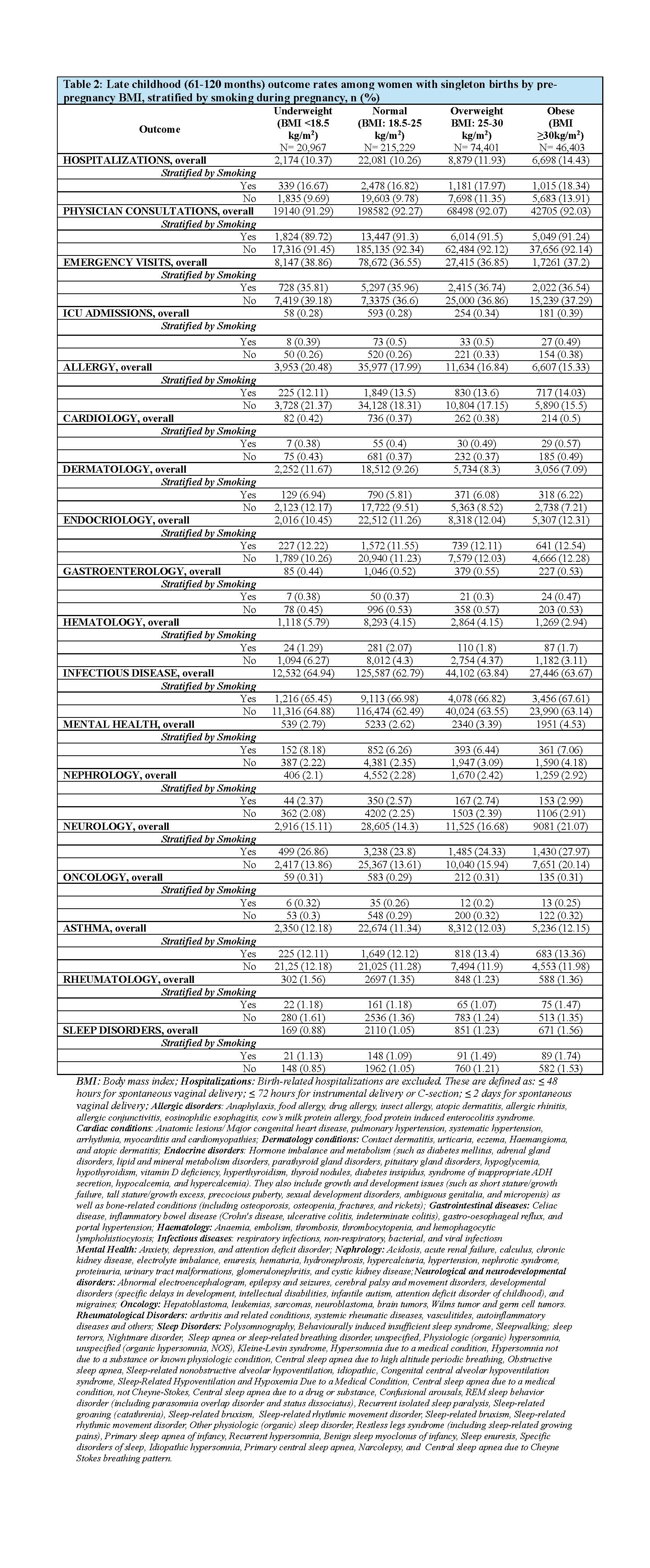
Strata specific adjusted risk ratios (ARRs) and 95% confidence intervals for the association between pre-pregnancy BMI and late childhood (61-120 months) health outcomes