Health Equity/Social Determinants of Health 10
Session: Health Equity/Social Determinants of Health 10
199 - Improving Screening and Documentation of Neonatal Adverse Childhood Experiences with Quality Improvement Methodology
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 199.5186
Kaitlyn Sacotte, University of Utah, Salt Lake City, UT, United States; Jane N. Nampijja, UoU, Layton, UT, United States; Carrie Torr, University of Utah School of Medicine, Salt Lake City, UT, United States

Kaitlyn Sacotte, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
University of Utah
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Social determinants of health (SDH) affect both short- and long-term neonatal outcomes. Childhood SDH include Adverse Childhood Experiences (ACEs). Neonatal ACEs (ACEs a baby is born with), are inconsistently screened for in the postnatal period. An analysis at our institution found only 2% of neonates admitted to the neonatal intensive care unit (NICU) were fully screened for ACEs. Without a complete ACEs screening, we are unable to evaluate the association between neonatal ACEs and outcomes.
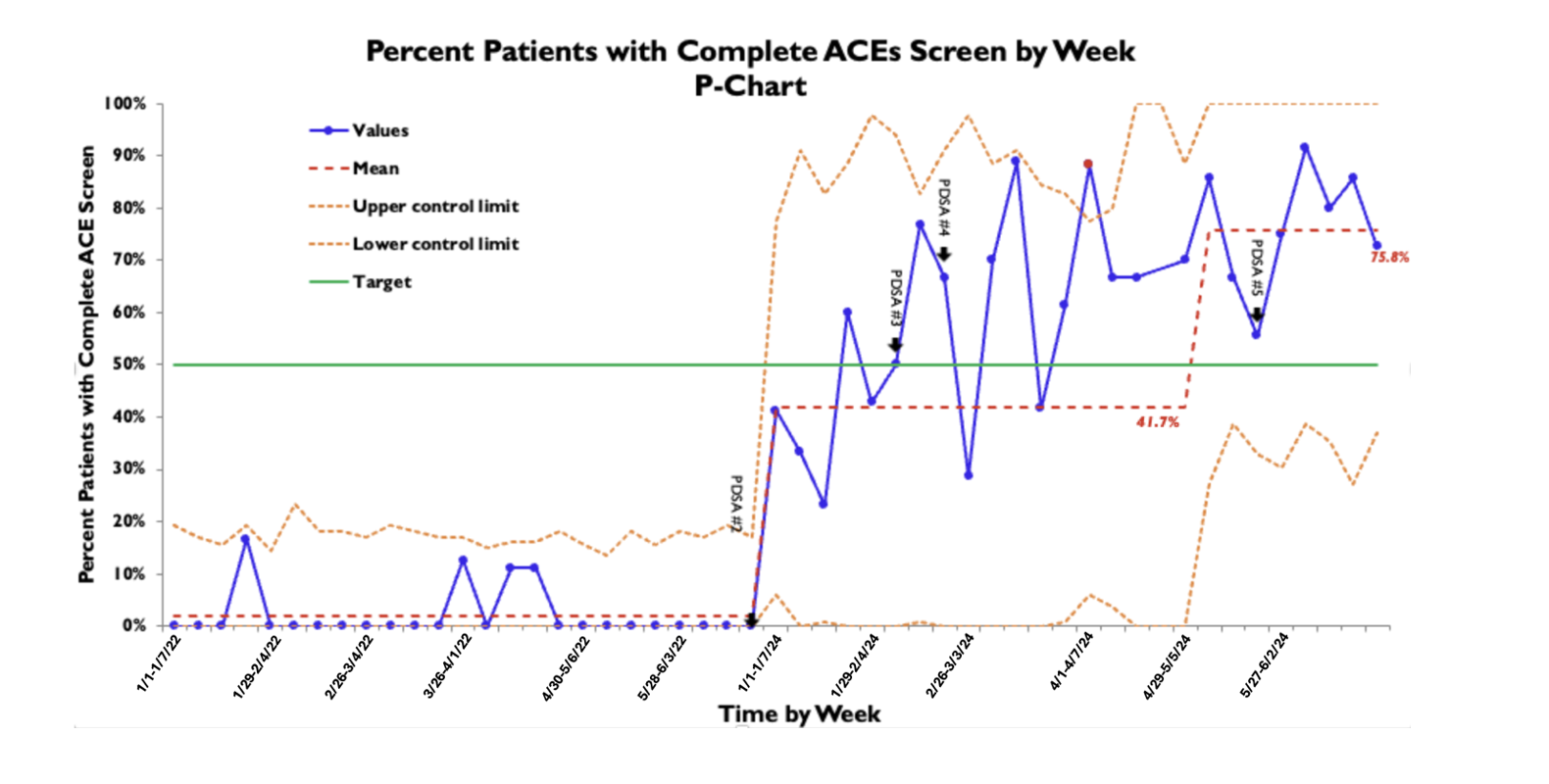
Objective: To improve screening and documentation of all five neonatal ACEs from 2% to 50% of all NICU patients by June 2024.
Design/Methods: In this IRB-exempt quality improvement project, all neonates admitted to the University of Utah Level III NICU from January 2022 to June 2024 were enrolled. Neonatal and maternal charts were reviewed for documentation of five ACEs: parental intimate partner violence, parental mental illness, parental incarceration, parental separation, and parental substance use. Using the Model for Improvement, we identified two key drivers of incomplete screening and focused on note templates in the electronic health record (EHR) as a high-priority leverage point. We defined the outcome measure as the percentage of patients with completely documented ACEs screening. Our process measure is the proportion of patients for whom the ACEs questionnaire is utilized, with balancing measures of perceived parental distress and absence of sensitive paternal information in maternal chart. We assessed the primary outcome using a P-chart.
Results: We have completed five plan-do-study-act (PDSA) cycles which included understanding social work screening process and documentation, implementing a ACEs screening tool within the EHR, increasing documentation via the ACEs tool through multiple process changes, and ensuring all staff were aware of the tool and importance of its use. We increased the proportion of patients with a complete ACEs screen documented from 2% to 76% (Graph 1). ACEs questionnaire was used in 188/261 (72%) of patients. No sensitive paternal information was included in maternal charts and no increase in perceived parental distress was noted. An unintended outcome was identifying our social work staffing was well below national standards.
Conclusion(s): An EHR ACEs screening tool, when delivered via a trained social work professional, is an effective and safe method to improve screening. With increased screening, we can study the association of neonatal ACEs, an important SDH, on neonatal outcomes. Additionally, we are able to advocate for increased social work support for our families.
Graph 1: P-chart of percent of patients with complete ACEs screen over time
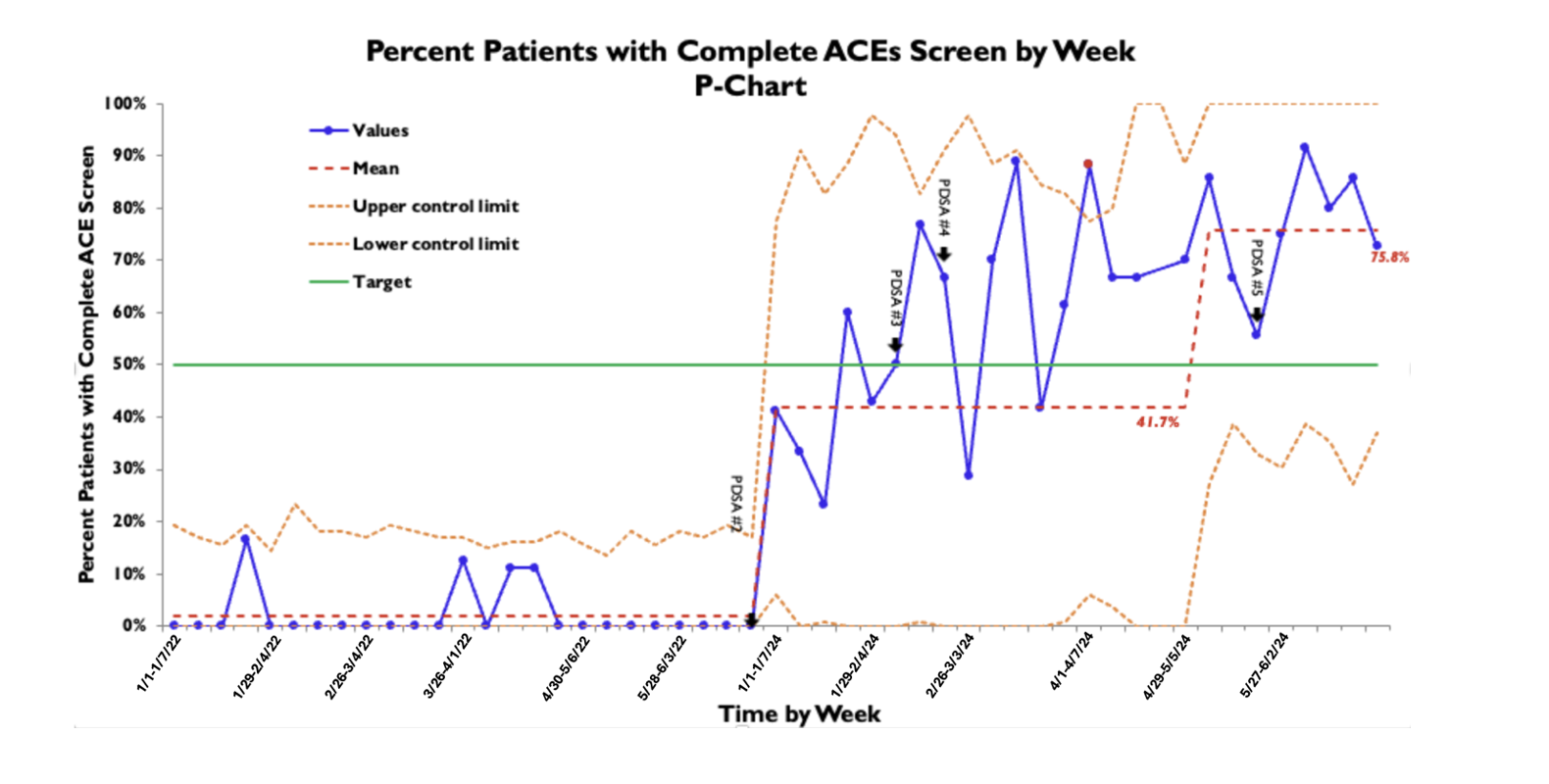 Each data point represents a week, with the first week of the month denoted with the date.
Each data point represents a week, with the first week of the month denoted with the date.Graph 1: P-chart of percent of patients with complete ACEs screen over time
 Each data point represents a week, with the first week of the month denoted with the date.
Each data point represents a week, with the first week of the month denoted with the date.

