Neonatal Hematology & Bilirubin Metabolism 1
Session: Neonatal Hematology & Bilirubin Metabolism 1
658 - Incidence of neonatal hyperbilirubinemia requiring intervention in non white term neonates receiving delayed cord clamping
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 658.5136
Mehwish Sheikh, University of illinois, Peoria, IL, United States; Shoji O. Samson, University of Illinois College of Medicine, Peoria, IL, United States; nabeeha S. khan, University of Illinois at Urbana-Champaign, Edwards, IL, United States
- MS
Mehwish Sheikh, M.D
Attending Neonatologist
University of illinois
Peoria, Illinois, United States
Presenting Author(s)
Background: The 2022 American Academy of Pediatrics (AAP) guidelines for the management of neonatal hyperbilirubinemia removed race as a risk factor. This is an initiative to move away from race-conscious medicine. However, little clarity is provided to encounter the differences due to genetic and sociocultural factors related to bilirubin metabolism. With delayed cord clamping ( DCC) widely practiced and the push for early discharges with little emphasis on a timely follow-up, the concern about rehospitalization is on the rise.
Objective: To examine the incidence of hyperbilirubinemia requiring intervention in nonwhite, term neonates, considering factors such as DCC, early discharge, and insufficient follow-up.
Design/Methods: We conducted a single-center retrospective chart review of newborns born at >36 weeks gestation who received DCC for >30 seconds and had a bilirubin level before discharge. Neonatal and maternal characteristics and identified risk factors (Table 1, Table 2) were collected. The primary outcome was the incidence of hyperbilirubinemia requiring intervention in the first seven days of life. The secondary outcome was peak serum bilirubin in the first 24 hours of life and hyperbilirubinemia
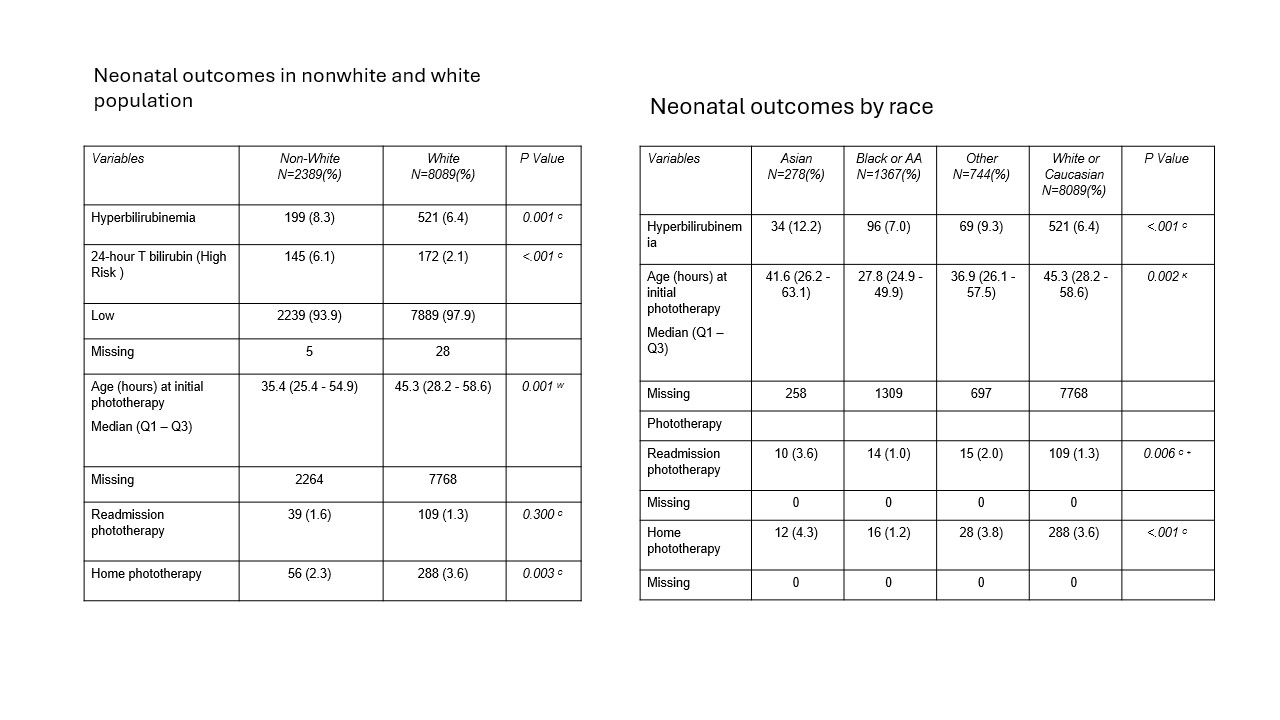
Results: Among 10,478 babies born after or at 36 weeks gestation who received DCC for >30 seconds, 22.8% were nonwhite, and 77.1% were white (Table 3) . The incidence of hyperbilirubinemia requiring phototherapy was 1.6% for Non-white and 1.3% for White (p=0.300). Non-white neonates had a higher rate of hyperbilirubinemia with an 8.3% (p-=0.001); however, after adjusting for all other risk factors, the adjusted odds ratio was 1.027 [95% CI: 0.845, 1.248] (p = 0.789). Hyperbilirubinemia requiring phototherapy occurred in 7.9% of Asian neonates. Asian neonates were 2.024 times more likely to develop hyperbilirubinemia than White neonates (p = 0.0002) (Table 3).
Conclusion(s): Our study concludes that there is no significant difference in hyperbilirubinemia requiring intervention between nonwhite and white neonates, taking into account factors such as DCC, early discharge, and insufficient follow-up. However, Asian neonates remain at a significantly higher risk for hyperbilirubinemia requiring phototherapy. Further research into genetic variations among at-risk populations is essential. Additionally, guidelines are needed to identify the at-risk groups, enabling healthcare providers to improve care while reducing racial disparities in outcomes.
Table 1 Neonatal and maternal characteristics
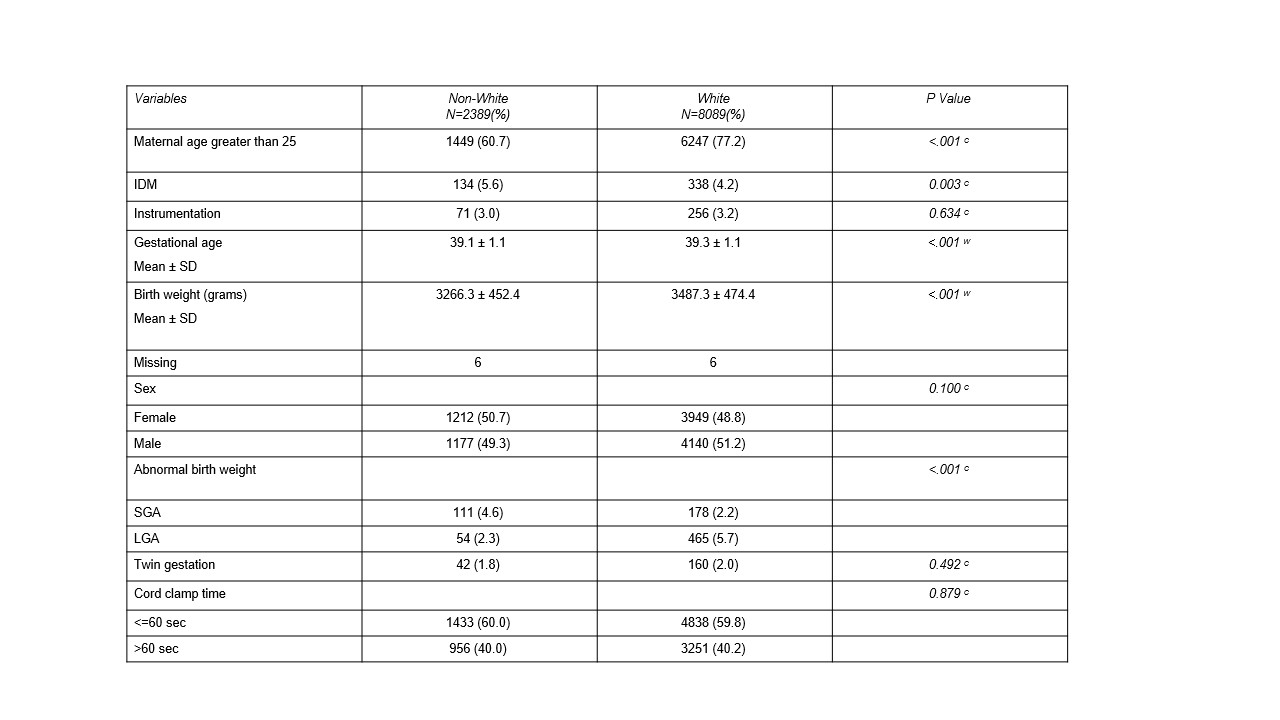
Table 2 Neonatal risk factors for hyperbilirubinemia
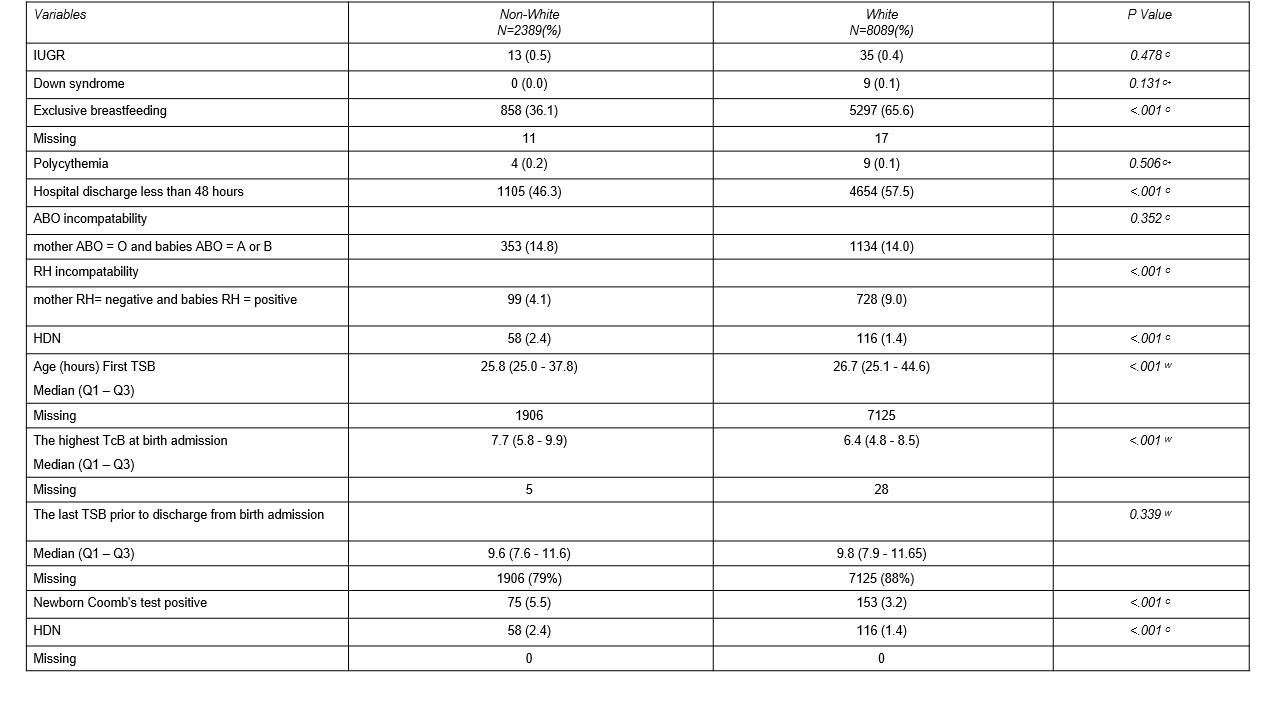
Table 3 - Neonatal outcome
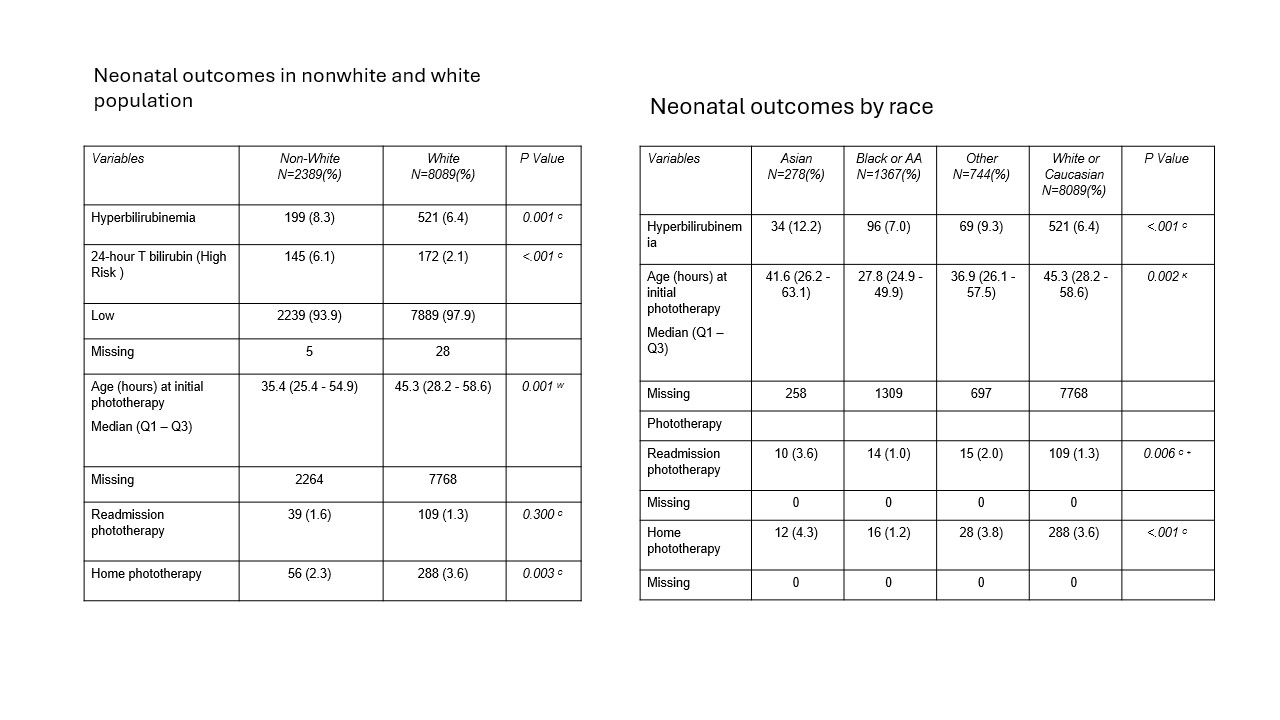
Table 1 Neonatal and maternal characteristics
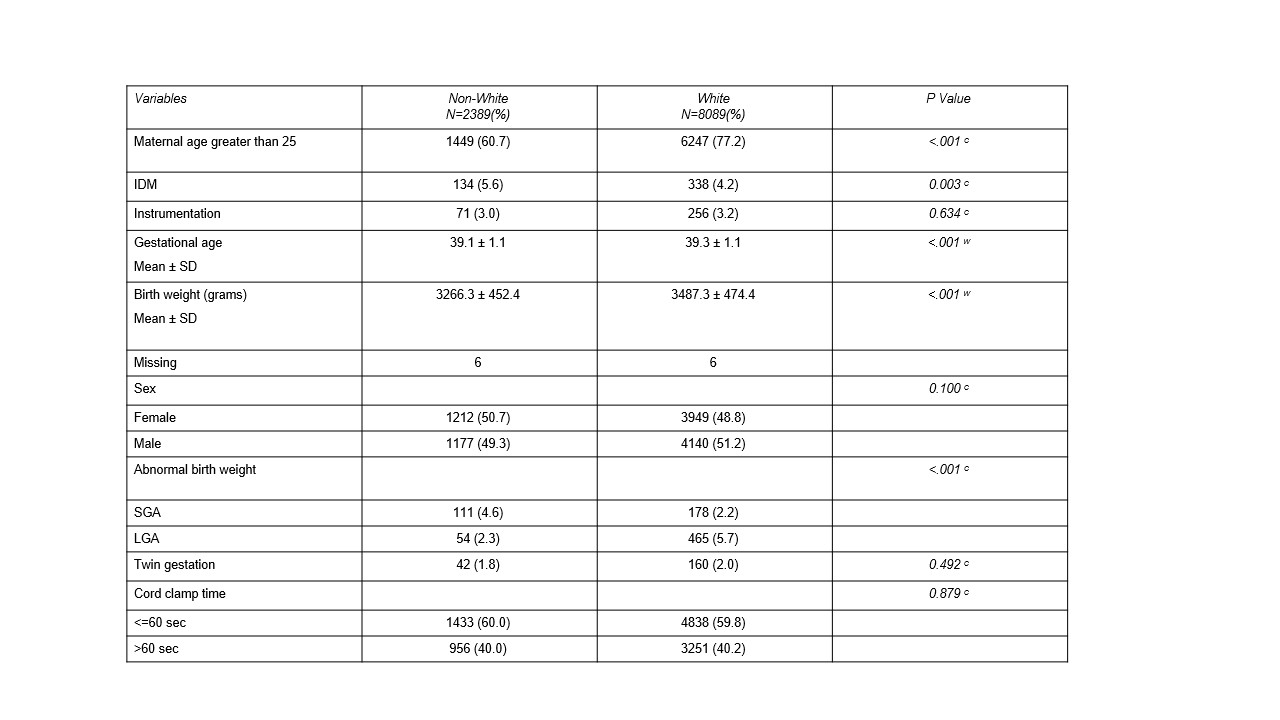
Table 2 Neonatal risk factors for hyperbilirubinemia
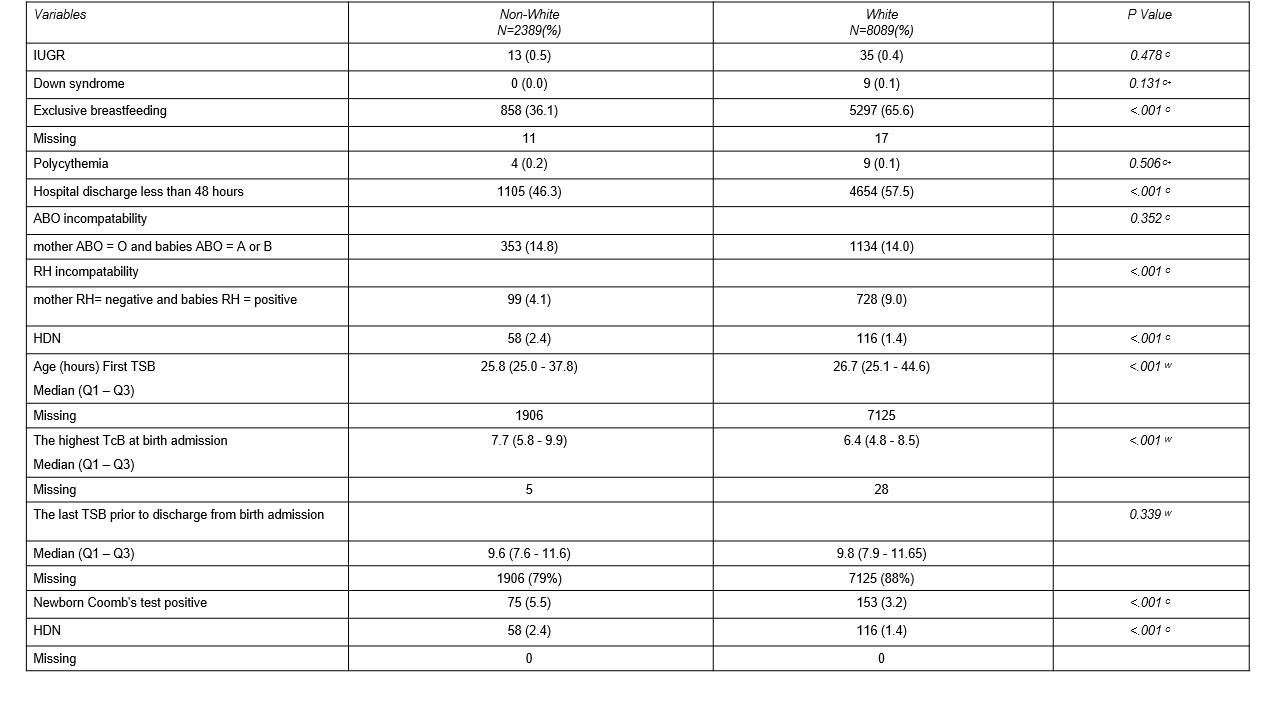
Table 3 - Neonatal outcome