Adolescent Medicine 6: Sexual & Reproductive Health
Session: Adolescent Medicine 6: Sexual & Reproductive Health
157 - Improving Resident Competency in Evaluating Menstrual Blood Loss Quantification
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 157.5156
Sarah Sabir, The Children's Hospital at Monmouth Medical Center, Long Branch, NJ, United States; Jonathan E. Teitelbaum, The Children's Hospital at Monmouth Medical Center, Long Branch, NJ, United States; Meenakshi Goyal-Khemka, Rutgers, Robert Wood Johnson Medical School, Plainsboro, NJ, United States; Anam Rafique, Shifa College of Medicine, ISLAMABAD, Islamabad, Pakistan; Narihan Osman, Unterburg childrens hospital, Scotch plains, NJ, United States
- SS
Sarah Sabir, MD
Resident
The Children's Hospital at Monmouth Medical Center
Long Branch, New Jersey, United States
Presenting Author(s)
Background: Heavy menstrual bleeding (HMB) is defined as menstrual blood loss over 80 mL per cycle, affecting quality of life and well-being of women. It is often underdiagnosed due to differences between perceived and actual blood loss. Methods to measure HMB, such as the Pictorial Blood Loss Assessment Chart (PBAC), have limitations. Many physicians are uncomfortable discussing menstrual health due to stigma and lack of training.
Objective: To improve comfort levels for diagnosing HMB and postpartum hemorrhage (PPH).
To improve awareness and use of tools e.g. PBAC.
Design/Methods: Residents from the Pediatrics, Internal Medicine (IM), and OB-GYN departments at Monmouth Medical Center participated in the study approved by the Institutional Review Board. They received an anonymous questionnaire developed by a pediatric hematologist, which was pilot-tested with seven physicians and revised for clarity. It included specialty and years of practice, comfort diagnosing HMB and PPH (Likert scale) and self-rated knowledge and experience quantifying HMB. It was followed by a lecture and lunch. A follow-up survey was sent three months later.
Results: Of the 71 residents emailed, 53 completed the pre-intervention questionnaire and 45 completed the post-intervention questionnaire. Analysis showed no significant change in overall comfort diagnosing HMB (p = 0.18) or primary and secondary PPH (p = 0.87 and 0.92 respectively) after the intervention. OB-GYN residents had higher baseline comfort compared to Pediatrics and IM. Post-intervention, Pediatrics and OB-GYN residents showed modest improvement, while IM residents showed minimal change. Comfort in diagnosing HMB increased with residency year, and PGY-3 residents showed the greatest improvement in diagnosing PPH. Tool awareness improved, especially for the PBAC, but this did not fully translate to increased usage, with only minor changes observed. OB-GYN residents' tool awareness and usage remained high with little change post-intervention.
Conclusion(s): Raising physician awareness of menstrual blood loss evaluation tools may improve early diagnosis of heavy menstrual bleeding and anemia, enhancing women's quality of life. Our intervention increased awareness, especially among non-OB-GYN residents, but tool usage remained low, revealing a gap between knowledge and practice. A single lecture was insufficient, highlighting the need for future QI efforts involving workshops, discussions, and simulations, along with more qualitative feedback and departmental collaboration.
Table 1 shows the breakdown of participants in the study
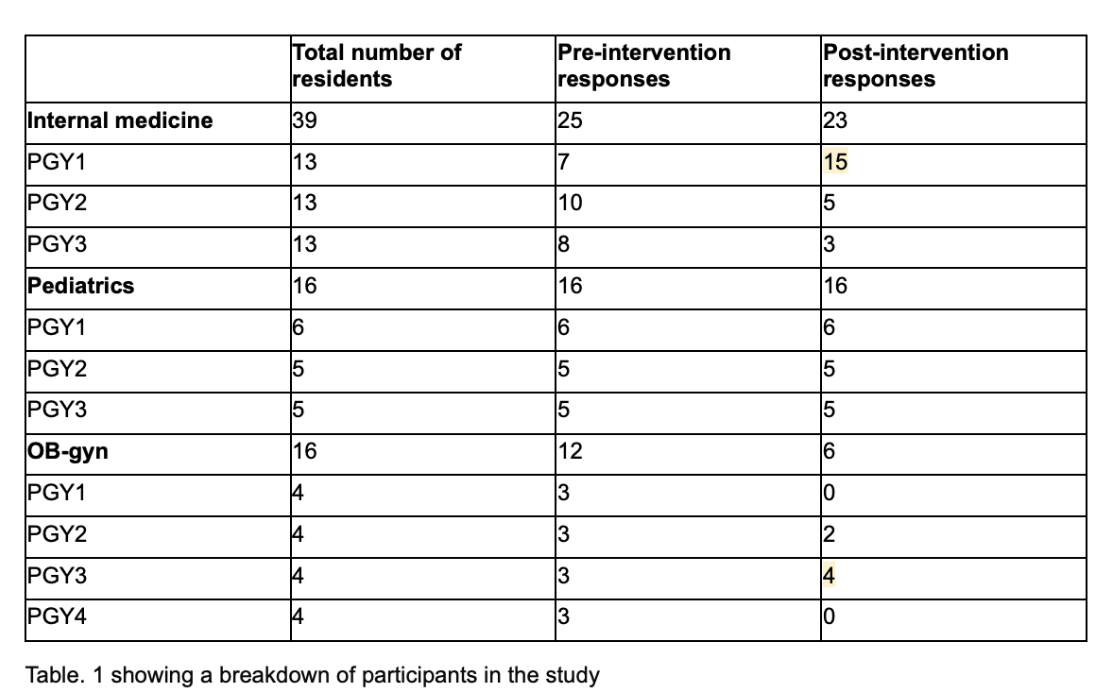 Table 1 shows the breakdown of participants in the study
Table 1 shows the breakdown of participants in the studyGraphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residency
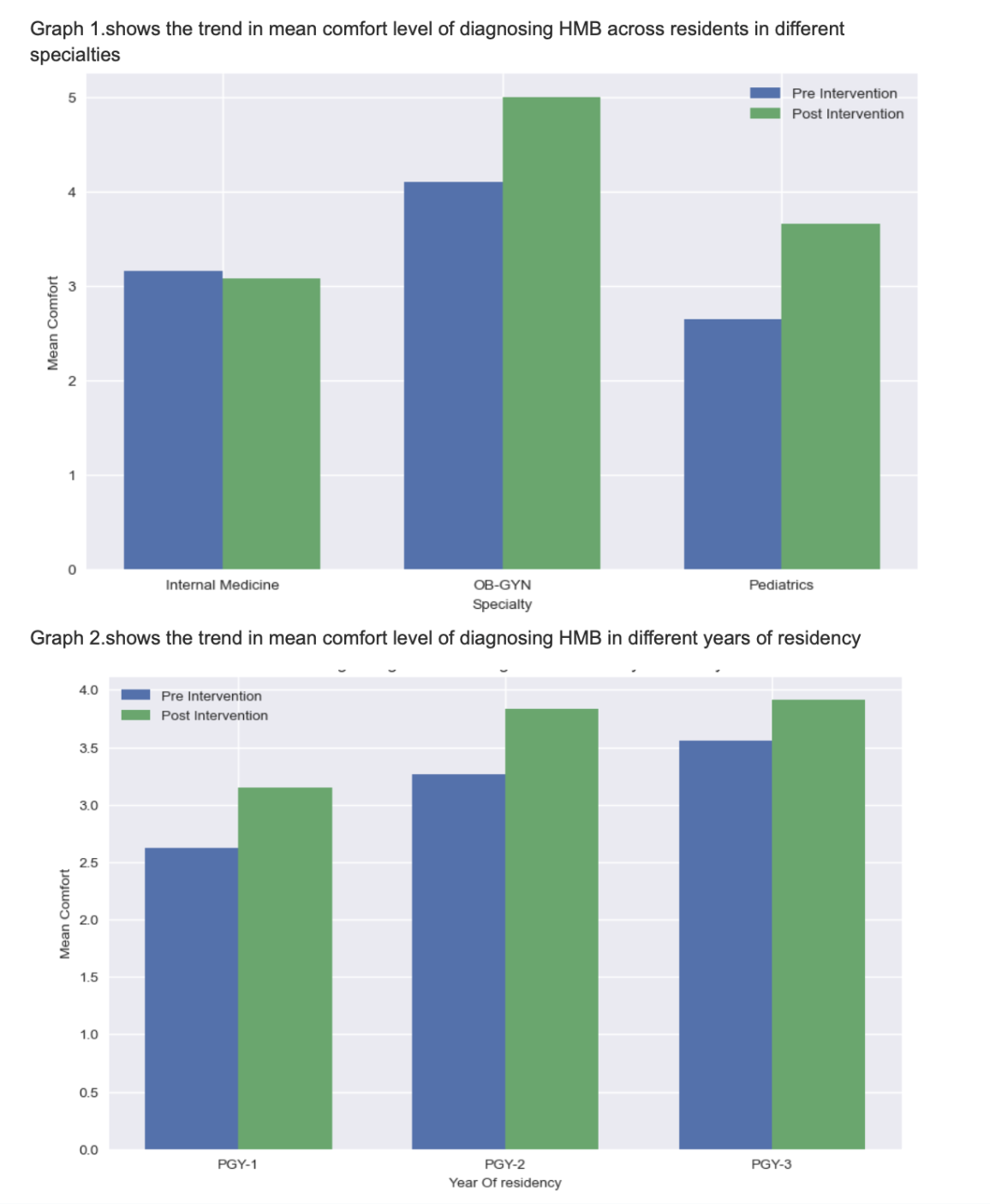 Graphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residency
Graphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residencyCharts 1 and 2 show the use of menstrual tools in the pre and post intervention survey
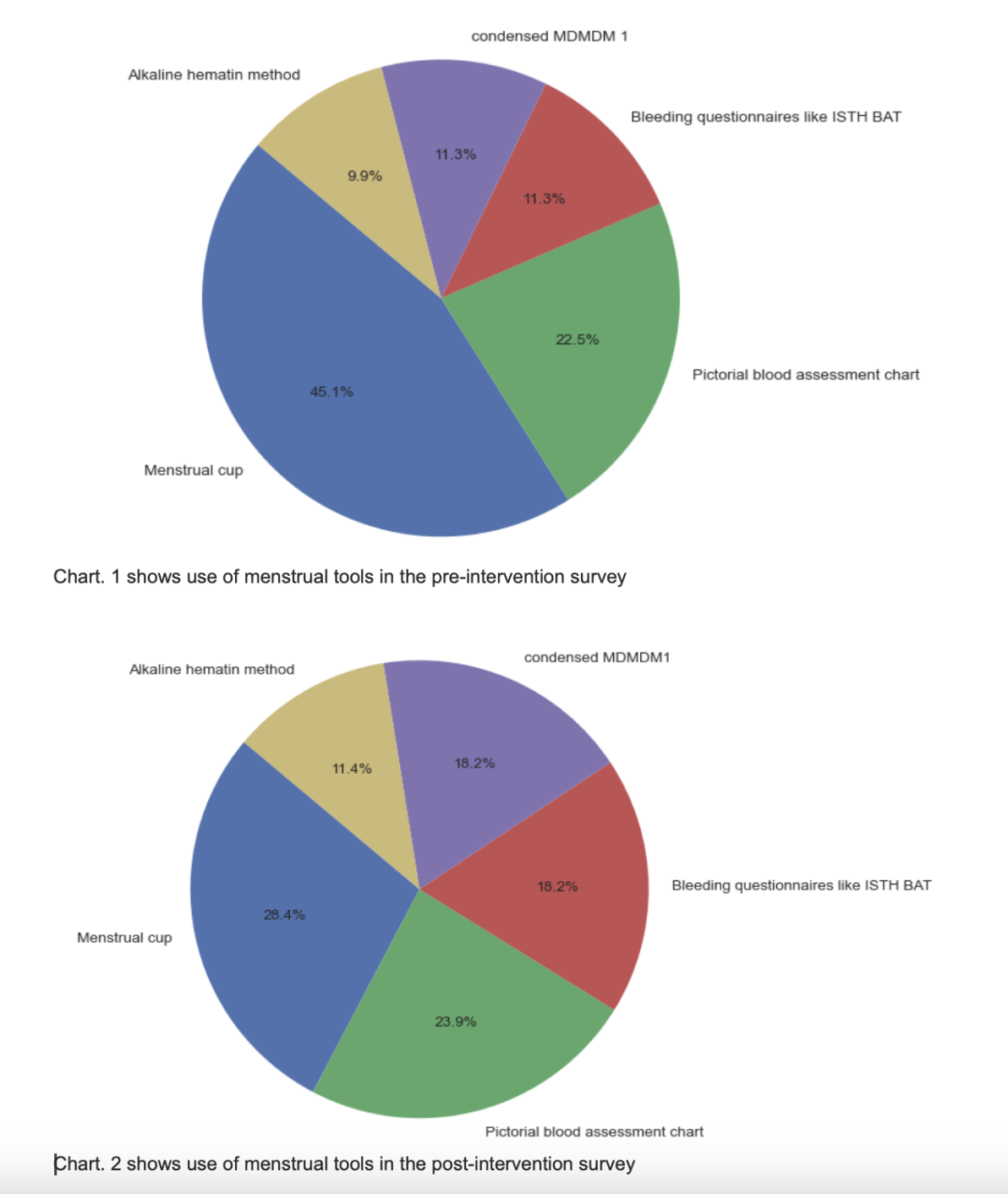 Charts 1 and 2 show the use of menstrual tools in the pre and post intervention survey
Charts 1 and 2 show the use of menstrual tools in the pre and post intervention surveyTable 1 shows the breakdown of participants in the study
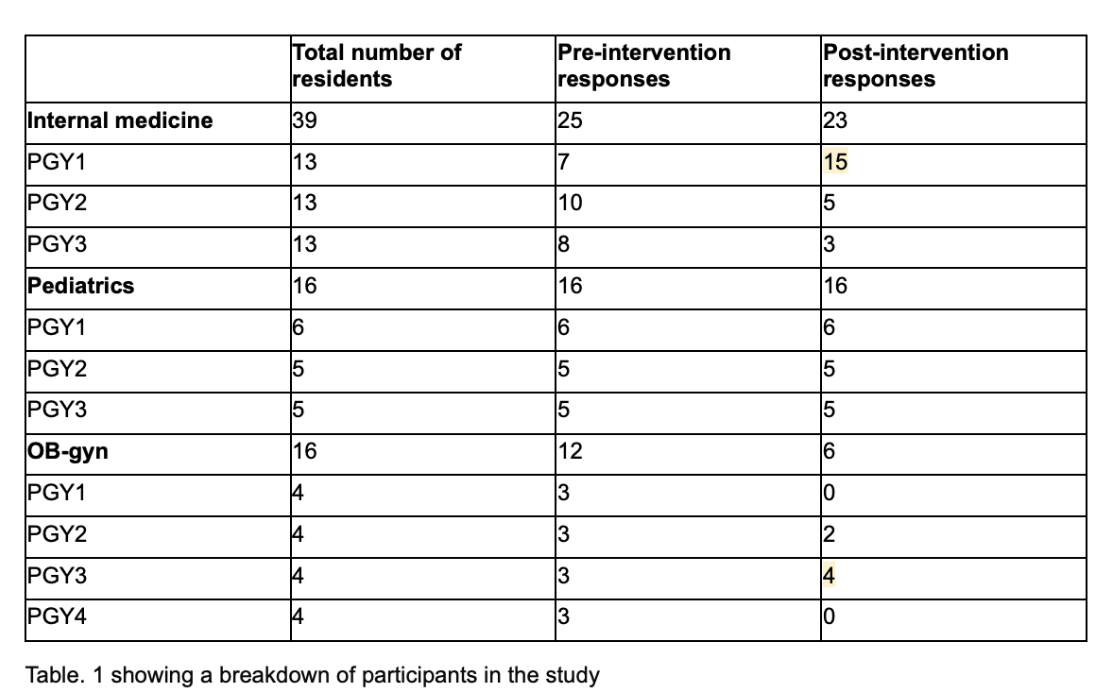 Table 1 shows the breakdown of participants in the study
Table 1 shows the breakdown of participants in the studyGraphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residency
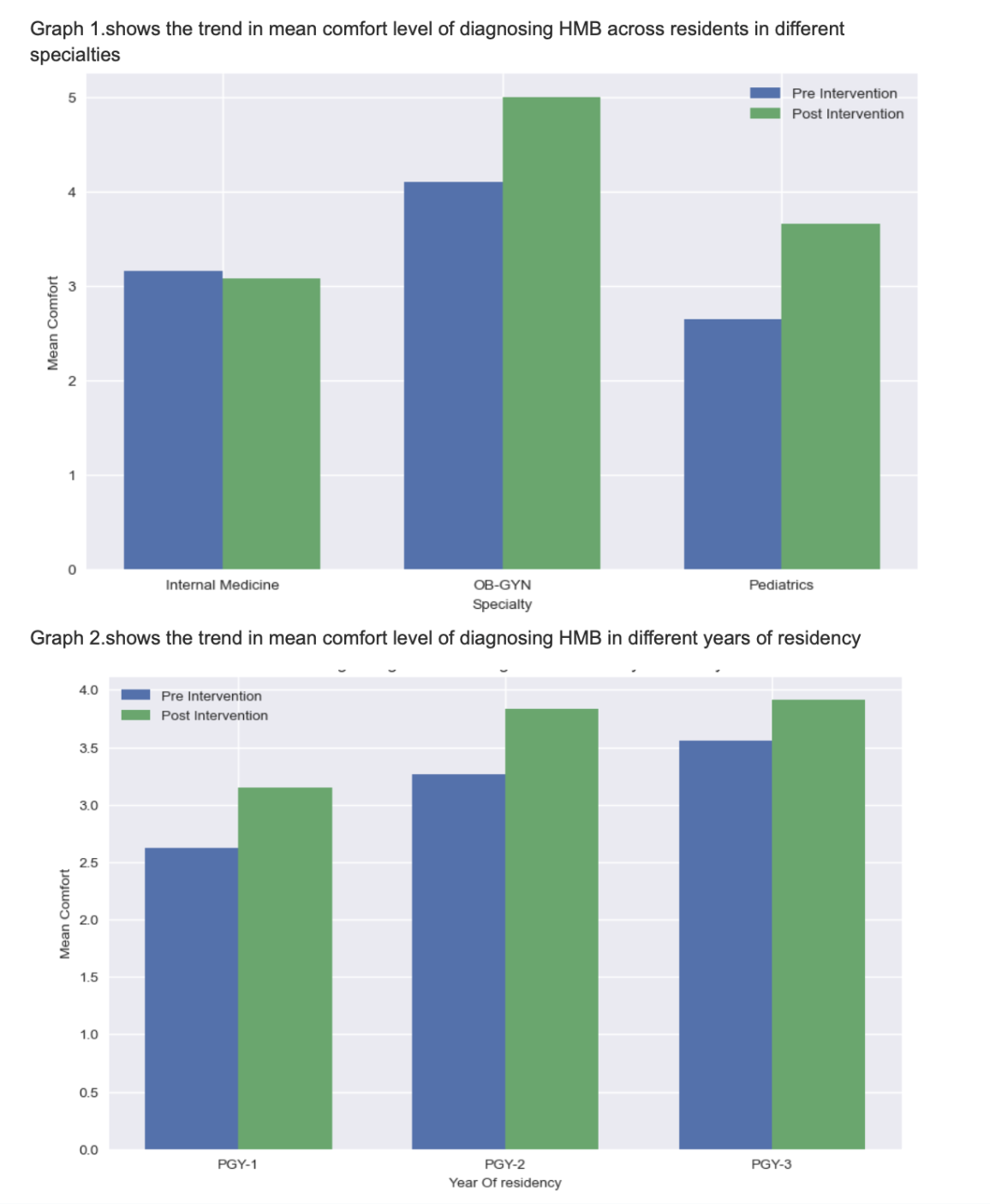 Graphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residency
Graphs 1 and 2 show the trend of mean comfort level of diagnosing HMB in residents across different specialties and years of residencyCharts 1 and 2 show the use of menstrual tools in the pre and post intervention survey
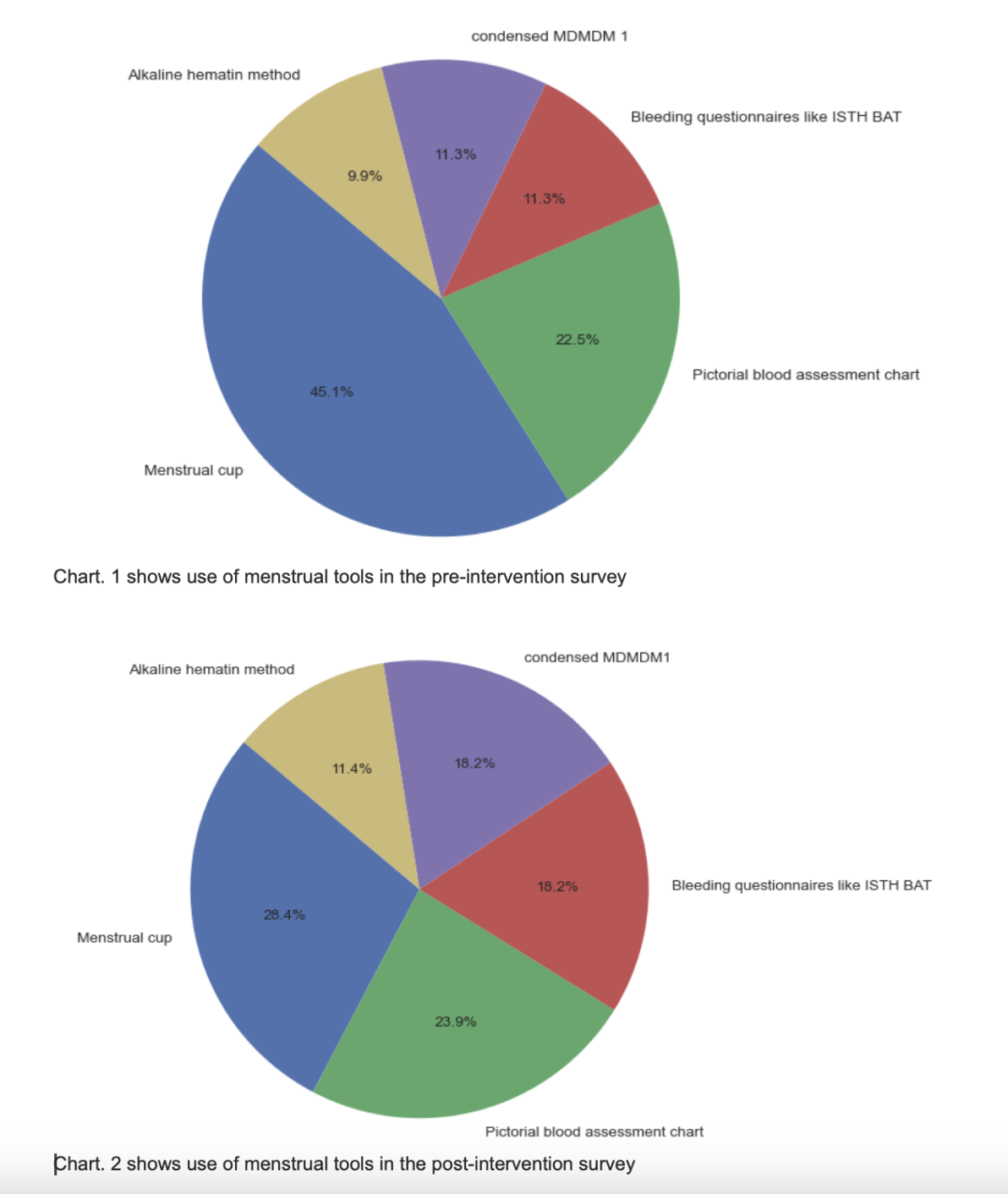 Charts 1 and 2 show the use of menstrual tools in the pre and post intervention survey
Charts 1 and 2 show the use of menstrual tools in the pre and post intervention survey
