Emergency Medicine 12
Session: Emergency Medicine 12
544 - Pediatric Emergency Department Burn Care Before and After Becoming a Burn Center
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 544.5589
Karna Mangrola, Wake Forest Baptist Health - Brenner Children's Hospital, Winston Salem, NC, United States; Amelia Davidson, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; James H. Holmes, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Milan Nadkarni, Wake Forest Baptist Health - Brenner Children's Hospital, Winston Salem, NC, United States

Karna Mangrola, DO (he/him/his)
Pediatric Emergency Medicine Fellow
Wake Forest Baptist Health - Brenner Children's Hospital
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: Pediatric burns represent a fifth of accidental injuries within the USA. Pediatric patients are a unique population regarding burns and their management. Currently, there are no standardized treatment approaches for pediatric burns. Our study looks at the impact becoming a burn center can have on interdisciplinary care of the acute pediatric burn patient.
Objective: Highlight the differences and outcomes in acute burn management for pediatric patients before and after becoming a level I burn center as it pertains to care within, and coordinated, by the emergency department.
Design/Methods: In collaboration with the Critical Illness, Injury and Recovery Center (CIIRC), an interdisciplinary cohort between emergency medicine, burn surgery, and the burn intensive care unit, data was extracted from a longitudinal burn database regarding pre-, intra-, and post-admission burn care. The electronic medical record was reviewed between the years 2008-2022 with focus on the following variables: demographics, acuity of presentation, mechanisms of injury, fluid resuscitation, disposition, and operative or non-operative goals. Injuries that were from chemical burns or ingestions, and charts that were inaccessible or incomplete were excluded.
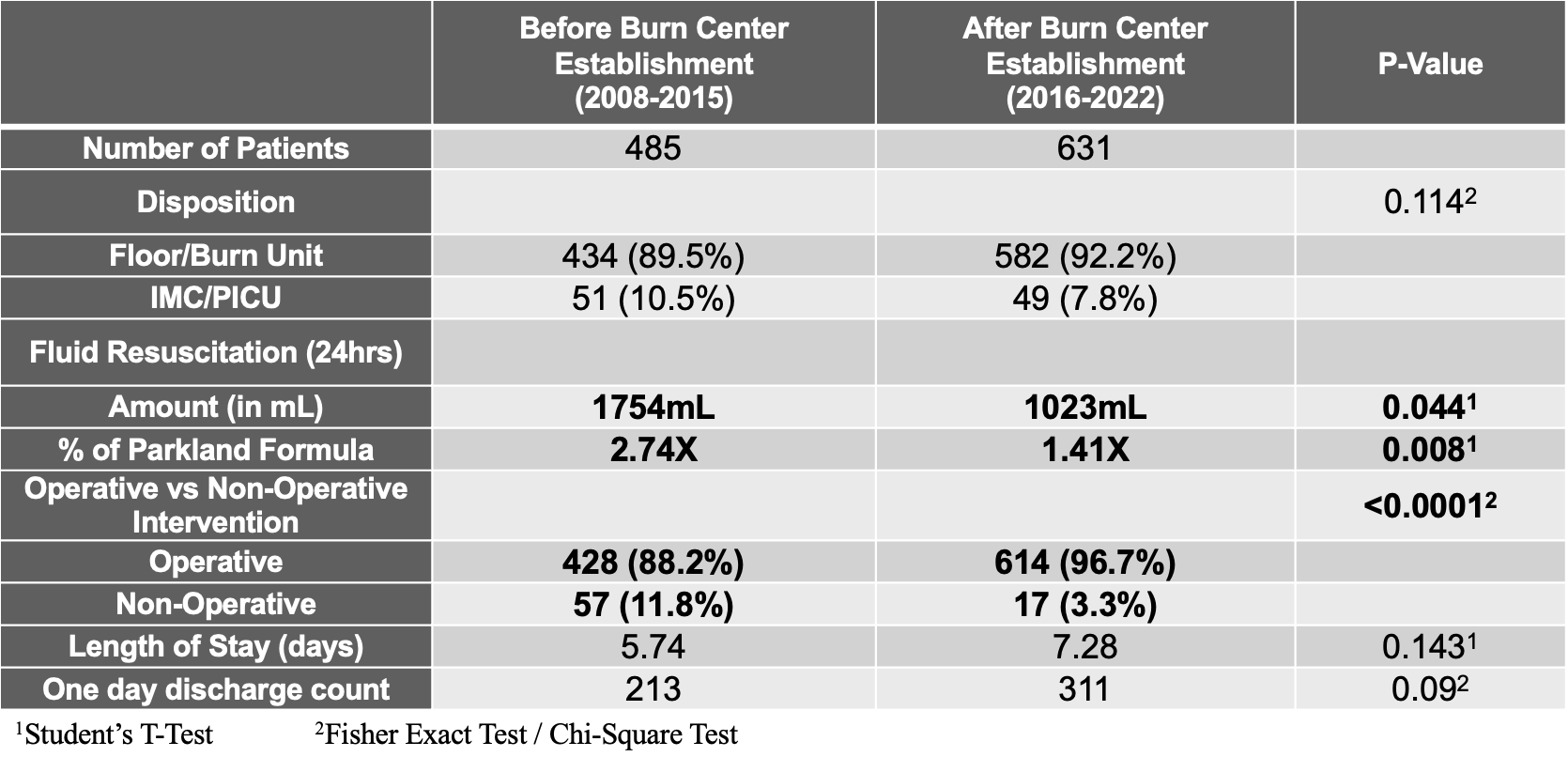
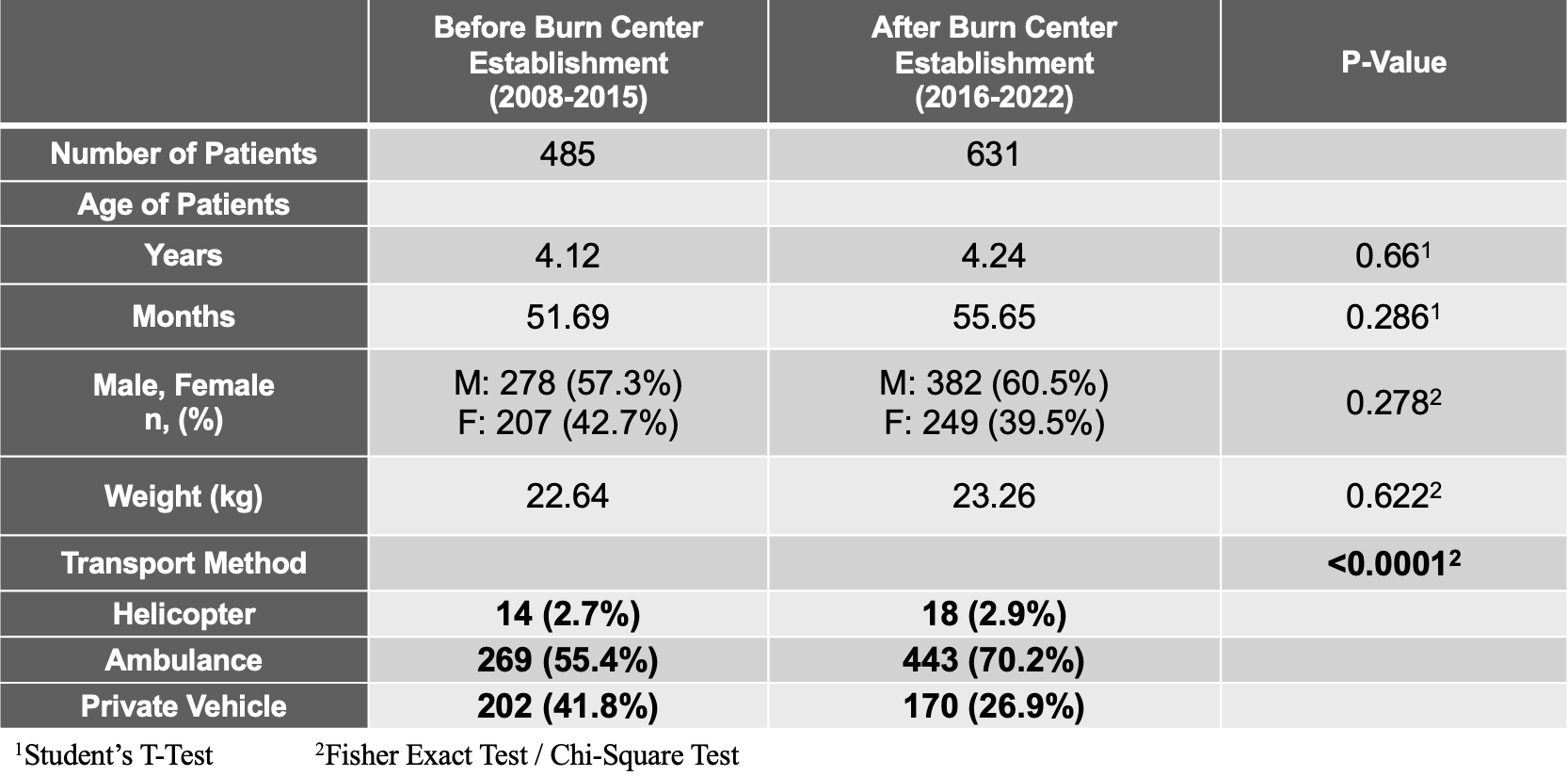
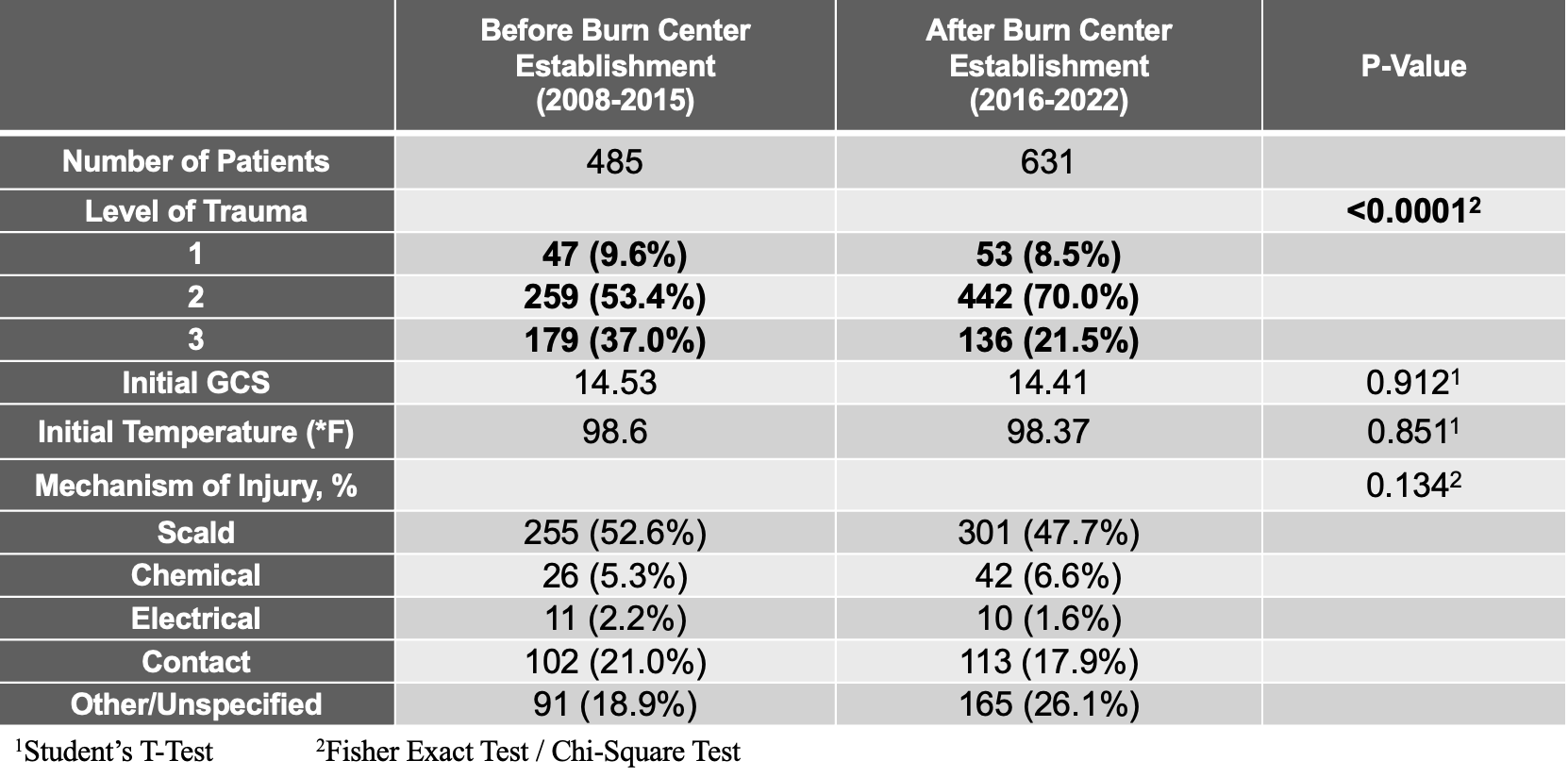
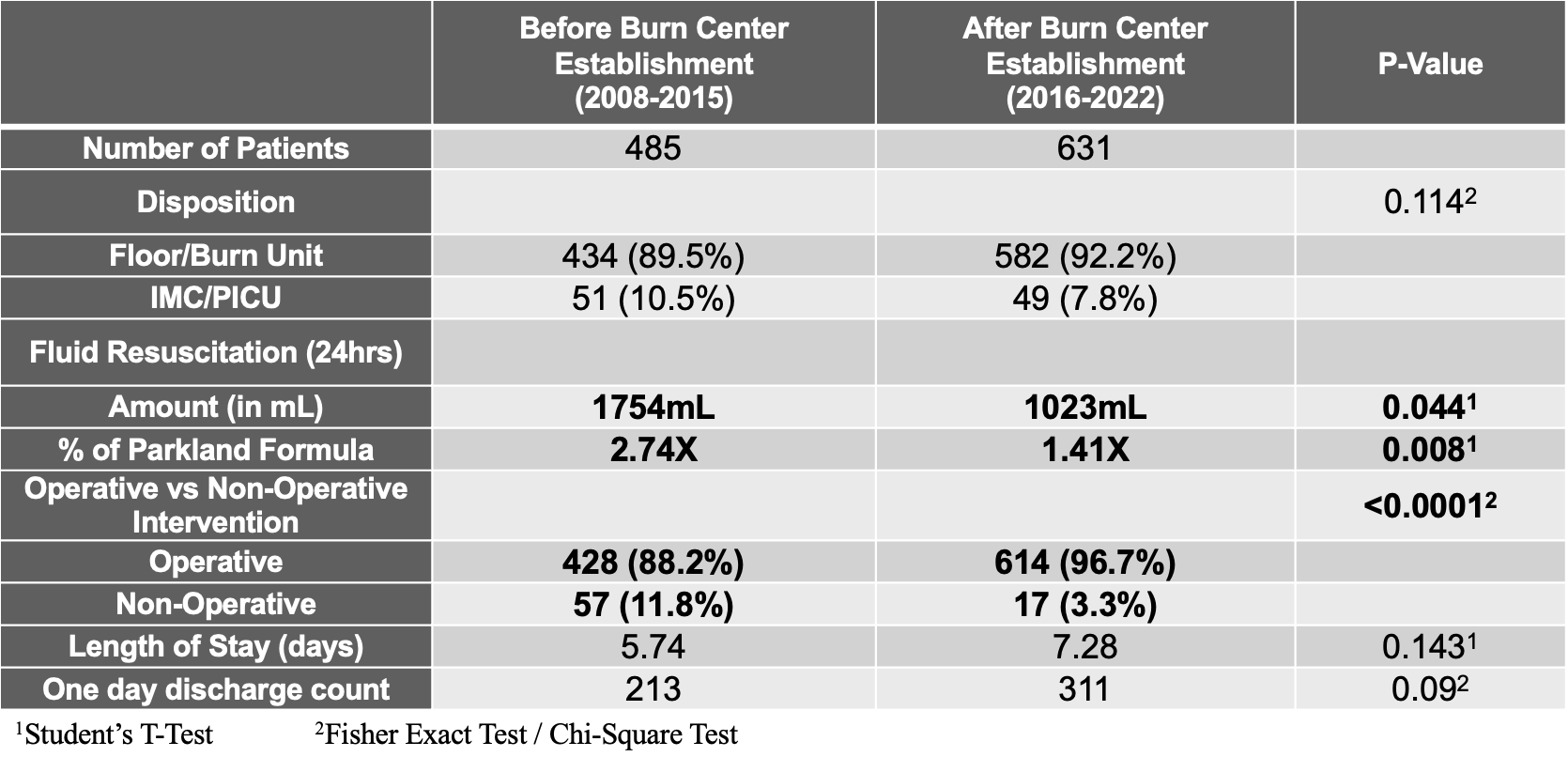
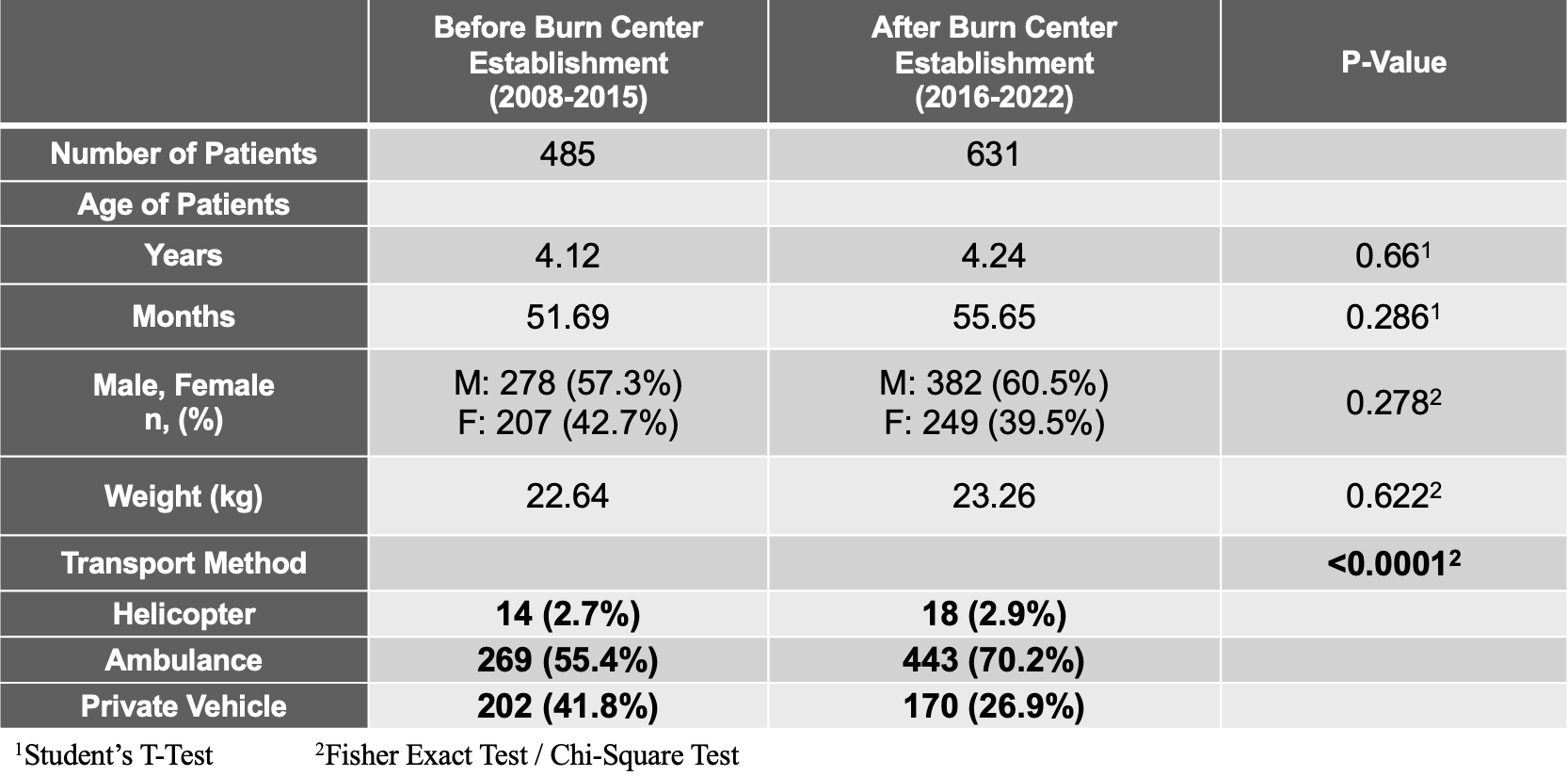
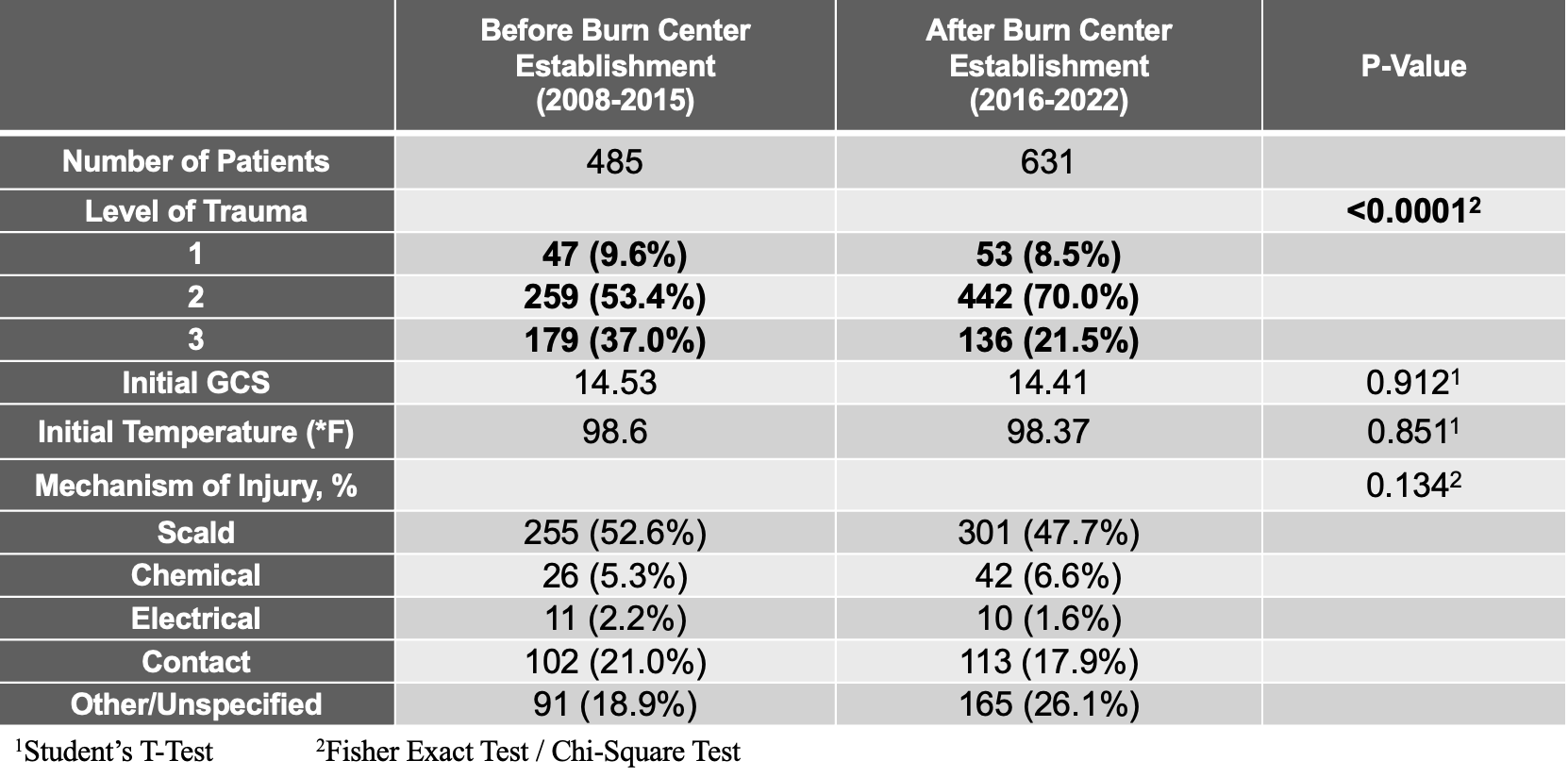
Results: 485 and 631 patients were included in the pre-burn center and post-burn center groups during the study period, respectively. Patient demographics were consistent between pre-burn center and post-burn center groups. Pediatric burn center designation led to better management of more severe (acute) burn injuries with improved fluid resuscitation accuracy. As before designation, there was fluid over resuscitation. After becoming a burn center, there was more accurate utilization of the Parkland formula (p < 0.05). Operative measures (such as debridement and grafting) saw an increase in utilization, 88.2% pre-burn center vs 96.7% post-burn center (p < 0.05). Additionally, there was an increase in appropriate inter-hospital transport of acute injuries, particularly with ambulances: 55.4% pre-burn center vs 70.2% post-burn center (p < 0.05) with a decrease in private vehicle use, 41.8% pre-burn center vs 26.9% post-burn center. However, there was no statistically significant changes in length of stay.
Conclusion(s): Pediatric burn center designation led to better management of burn injuries with increased appropriate transfer rates, more accurate fluid resuscitation and improved operative measures.
Demographics
Burn Leveling
Burn Management from ED
Demographics
Burn Leveling
Burn Management from ED