Mental Health 4
Session: Mental Health 4
101 - Outpatient Follow up After a Mental and Behavioral Health Visit to an Urban Pediatric Emergency Department
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 101.5765
Nirupama Kannikeswaran, Central Michigan University College of Medicine, Detroit, MI, United States; Sam M. Streberger, Children's Hospital of Michigan, Detroit, MI, United States; Anika Sood, Children's Hospital of Michigan, Detroit, MI, United States; Joshua Prabhu, Children's Hospital of Michigan, Bloomfield Hills, MI, United States
- NK
Nirupama Kannikeswaran, MBBS (she/her/hers)
professor of pediatrics and emergency medicine
Central Michigan University College of Medicine
Detroit, Michigan, United States
Presenting Author(s)
Background: There has been a significant increase in mental and behavioral health (MBH) visits to pediatric emergency departments (PED). The National Child Core Set of quality measures recommends an outpatient MBH follow-up visit within 7 and 30 days for children 6-17 years of age. Outpatient follow-up rates
and barriers to the recommended follow-up have not been well studied in racial and ethnic minority children.
Objective: Our objectives were to describe the rate of and barriers to 7- and 30-day outpatient follow-up after a MBH visit to an urban PED.
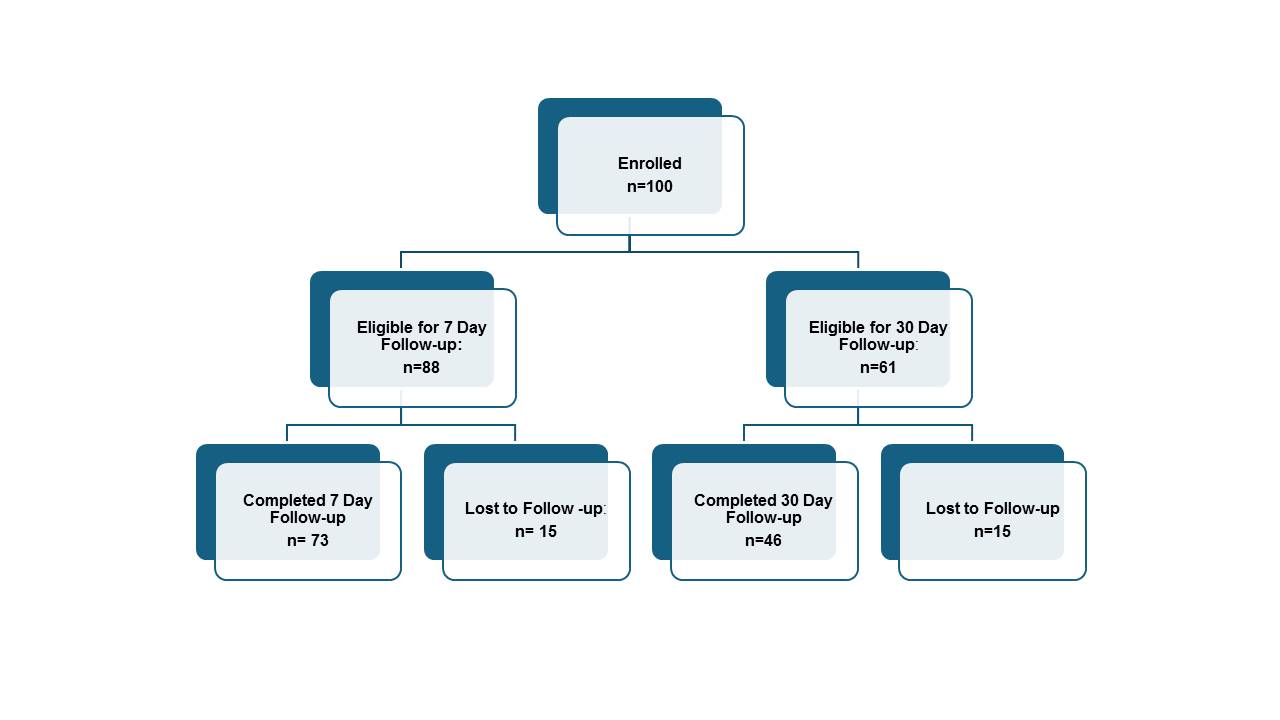
Design/Methods: We conducted a single center prospective cohort study of children aged 6-17 who presented for a MBH complaint to an inner-city PED. We abstracted patient demographics, MBH diagnosis, comorbid medical conditions, prior PED MBH visits and inpatient psychiatric hospitalizations, and PED disposition. A follow-up phone call was performed at 7 and 30 day to evaluate compliance with the recommended outpatient follow-up and parental barriers to follow-up.
Results: Of the 100 patients evaluated, majority were female (56;56%), non-Hispanic Black (75;75%) and had public insurance (73;73%). Depressive disorders were the most common diagnosis (40;40%) with one fifth (19, 19%) endorsing a prior suicide attempt and one third (30;30.9%) having a prior MBH PED visit or hospitalization. Of the 73 patients who completed the 7-day follow-up, one third (17; 23.2%) had not completed the recommended follow-up appointment and an additional 17 (23.2%) had not been evaluated despite setting up an appointment. Very few parents ( < 10%) reported financial, transportation, lack of knowledge about setting up the clinic appointment or distance to the clinic as barriers to setting up the follow -up appointment. Those with public insurance and who identified themselves as Non-Hispanic Black were less likely to have a follow-up appointment completed while those with depressive disorders were more likely to have had a follow-up appointment completed. Of the 46 patients who completed the 30 day follow up phone call, 7(15.2%) had still not had a follow-up appointment and an additional six (13%) patients had not been evaluated despite setting up a follow-up appointment. Six patients (13%) had a return visit to the PED for MBH complaint during the 30-day following the initial PED visit.
Conclusion(s): Despite few parents reporting barriers, nearly one third of the patients do not receive the recommended 7 day or 30 day follow-up after a PED MBH visit. Targeted interventions that increase access to timely outpatient follow-up can improve patient outcomes and reduce return visits to ED for MBH.
Fig. Study Flow Chart