Technology 4
Session: Technology 4
306 - Mixed Reality Technology in Neonatal Care: Initial experience in Brazil
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 306.5836
Danieli M. K.. Leandro, Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, Sao Paulo, Brazil; Patrik Gonçalves Rodrigues, Protecting Brains & Saving Futures, São Paulo, Sao Paulo, Brazil; Silvia Schoenau de Azevedo, Protecting Brains and Saving Futures, São Paulo, Sao Paulo, Brazil; Marcelo J.. Mimica, Santa Casa de Sao Paulo School of Medicine, Sao Paulo, Sao Paulo, Brazil; Bruno F. Anjos, PBSF- Protecting Brains and Saving Futures, São Paulo, Sao Paulo, Brazil; Valerie Y.. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States; Krisa P. Van Meurs, Stanford University, Palo Alto, CA, United States; Gabriel F. T. Variane, Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, Sao Paulo, Brazil
Danieli M. K Leandro, MD (she/her/hers)
Neonatologist
Irmandade da Santa Casa de Misericórdia de São Paulo
São Paulo, Sao Paulo, Brazil
Presenting Author(s)
Background: Mixed reality (MR) technology enables the interaction between elements of the real and virtual worlds, emerging as a tool that allows users to interact with virtual cues to assist with tasks encountered in the physical environment. This holographic-based technology is a potential tool to support real-time patient care. However, limited investigation exists in neonatal care. Further research is warranted to understand the potential of MR technology in neonatal care.
Objective: To assess the preliminary implementation of an MR tool as part of NICU care in a middle-income country.
Design/Methods: As a pilot, proof-of-concept investigation, nine neonatology fellows at a publicly funded, university-affiliated Brazilian hospital received 90 minutes of training on an MR-based device and software (NeonLens, Microsoft HoloLens 2, Redmond, Washington). The MR tool was piloted between May and September 2024 in the following scenarios: (1) daily sign-out rounds and clinical case discussions, in which the MR user communicated with a remotely located senior neonatologist who had access to the user’s viewpoint and audio, and (2) during the Modified Sarnat exam, in which the MR user had access to holographically presented instructions and multimedia resources to aid in the examination, along with remote video communication with an expert physician (assisted guided support) (Figure 1). As this was a pilot study, user experience was recorded qualitatively via a survey, and no patient outcome data were collected.
Results: The MR tool was used in 45 sign-out rounds or clinical case discussions with remote experts and 12 Modified Sarnat exams, totaling 34 hours of use. Overall, the survey respondents highlighted the benefit of having a remote expert, streamlining the performance of sign-out rounds, and the user-friendly interface that provided easy access to feedback on the Modified Sarnat exam. Repeated use documented greater confidence and ease in using the MR tool. The main challenge was that bedside nursing providers were not able to hear or participate in the interaction with the remote team during sign-out rounds.
Conclusion(s): MR’s ability to holographically provide protocol instructions, reference media, and enable first-person video communication with a remote expert highlights the potential of MR as a tool during bedside sign-out rounds, clinical case discussions, and education on the modified Sarnat exam. In addition, MR has the potential to decrease variability in neonatal care and deliver expertise to remote and low-resource settings.
Applications of NeonLens in neonatal care.
.png)
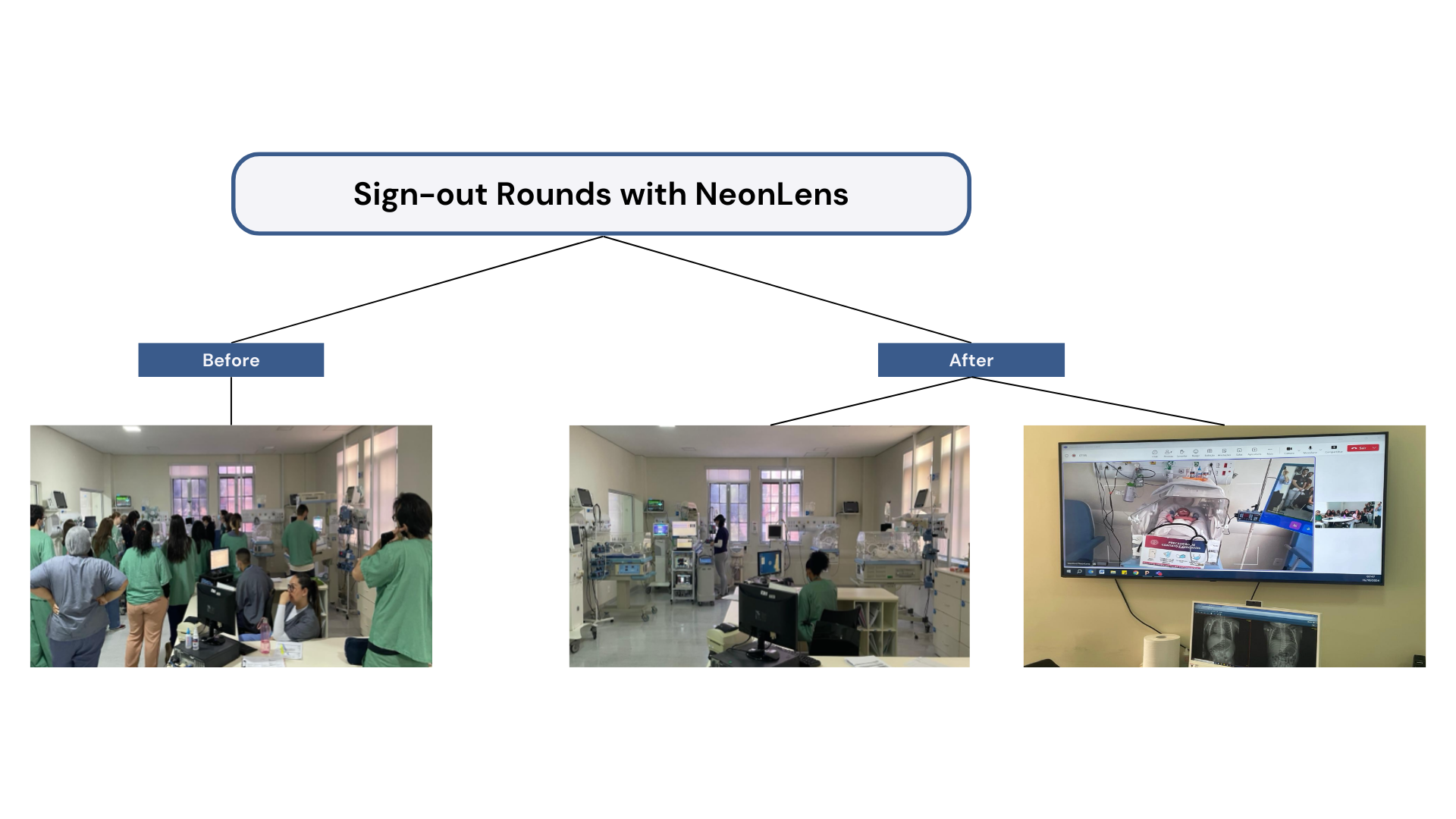
Impact of NeonLens during sign-out rounds.