Critical Care 4
Session: Critical Care 4
506 - Safety and Feasibility of Early Mobility in Pediatric ECMO Patients
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 506.6117
Alyssa Mueller, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Brian Bridges, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Melissa Danko, CHOA/Emory University, Atlanta, GA, United States; Daphne C. Hardison, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Katherine Hedden, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Alexandria N. Lawrence, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Kristina A. Betters, Vanderbilt University School of Medicine, Nashville, TN, United States

Alyssa Mueller, MD (she/her/hers)
Resident
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background: Early mobility (EM) has known benefits for critically ill pediatric patients including improved strength and mobility, decreased rates of delirium, positive parental and child experience during hospitalization, and reduction of hospital length of stay. Current guidelines recommend performing EM as the standard of care for all pediatric ICU (PICU) patients. However, until recently, patients on extracorporeal membrane oxygenation (ECMO) have been largely excluded from EM trials due to potential safety and feasibility concerns.
Objective: To establish safety and feasibility of a progressive early mobility protocol in pediatric patients on ECMO in a single center academic PICU.
Design/Methods: Retrospective data were collected and analyzed for all patients ages 0-18 years who required ECMO over a 6-year period following implementation of a progressive multi-disciplinary early mobility protocol (in which mobility activities are defined as levels I-III based on patient acuity and developmental age and can be progressed with stability and tolerance of lower levels). Additionally, a subset of patients requiring ECMO for 10 days or greater, termed long duration ECMO patients, were analyzed separately.
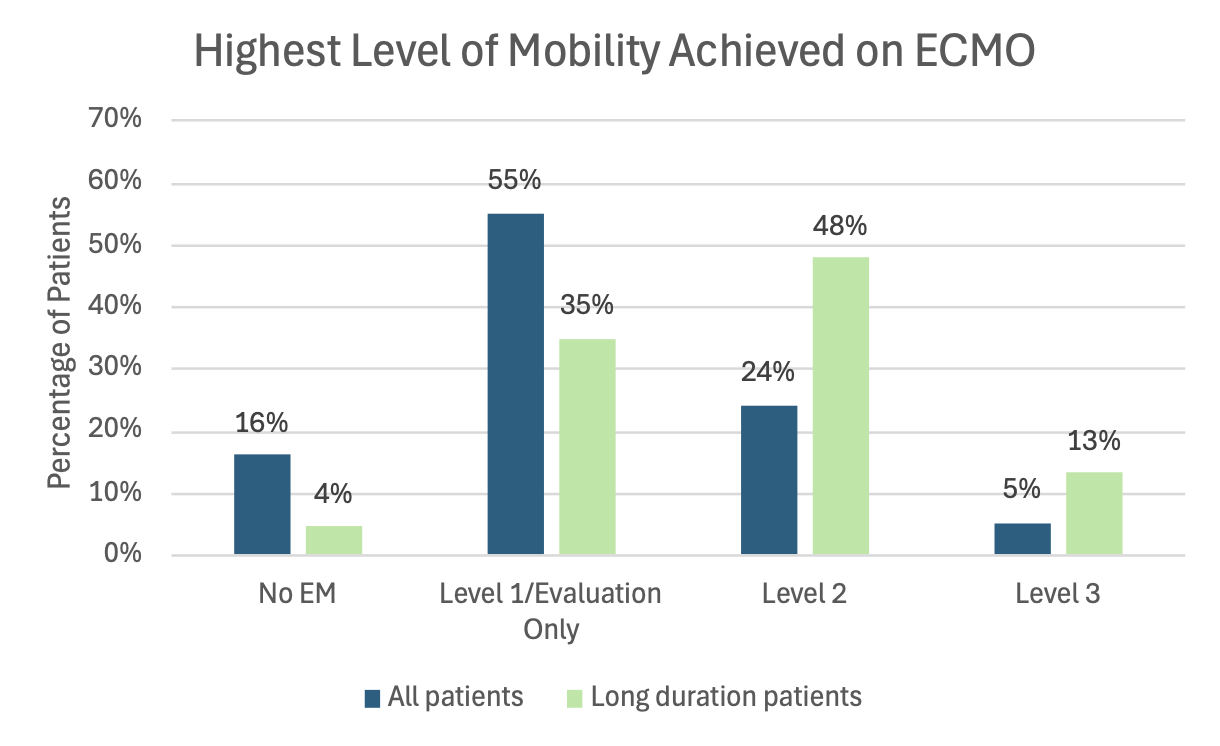
Results: Data was collected on a total of 62 patients. Eighty-four percent of these patients were able to participate in EM while on ECMO with 29 percent achieving at least level II activity and five percent achieving level III activity. Of 23 long duration ECMO patients, 61 percent of patients achieved level II activity and 13 percent of patients achieved level III activity. Of 297 EM sessions reviewed, signs of intolerance occurred in only six percent of sessions. No EM attributable serious adverse events occurred. However, an EM session did lead to recognition of neurologic exam changes and new diagnosis of a stroke in one patient.
Conclusion(s): Our data demonstrate that with a defined protocol and support of a multidisciplinary team, early mobility is safe and feasible for pediatric ECMO patients.
Patient demographics and key outcomes.
.png) ECMO = extracorporeal membrane oxygenation, PT = physical therapy, OT = occupational therapy, FSS = fatigue severity scale, PAMS = physical abilities and mobility scale
ECMO = extracorporeal membrane oxygenation, PT = physical therapy, OT = occupational therapy, FSS = fatigue severity scale, PAMS = physical abilities and mobility scaleHighest Level of Mobility Achieved on ECMO
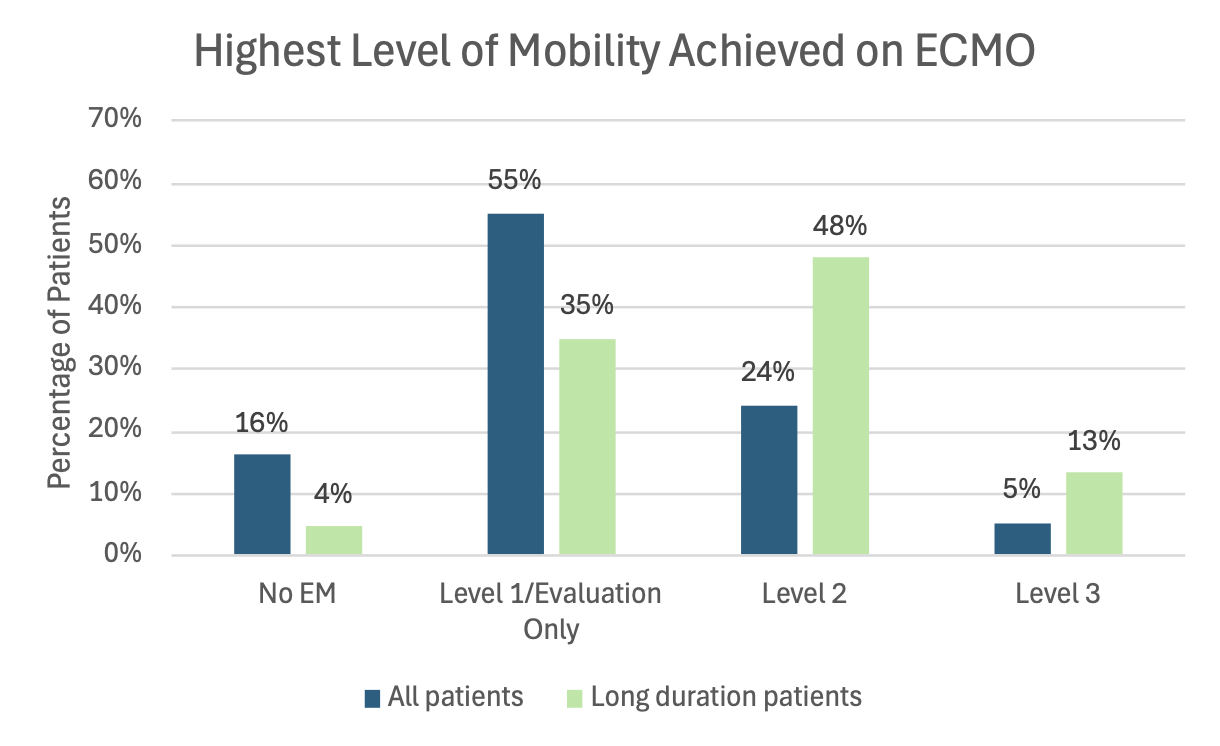 Levels based on institutional protocol.
Levels based on institutional protocol. Patient demographics and key outcomes.
.png) ECMO = extracorporeal membrane oxygenation, PT = physical therapy, OT = occupational therapy, FSS = fatigue severity scale, PAMS = physical abilities and mobility scale
ECMO = extracorporeal membrane oxygenation, PT = physical therapy, OT = occupational therapy, FSS = fatigue severity scale, PAMS = physical abilities and mobility scaleHighest Level of Mobility Achieved on ECMO
 Levels based on institutional protocol.
Levels based on institutional protocol. 
