Children with Chronic Conditions 4
Session: Children with Chronic Conditions 4
481 - Provider perspectives on complex care and palliative care collaboration for children with medical complexity
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 481.6118
Paul G. DiDomizio, Medical College of Wisconsin, Milwaukee, WI, United States; Madeline Johnson, University of Wisconsin-Milwaukee, Milwaukee, WI, United States; Annie B.. Friedrich, Medical College of Wisconsin, Milwaukee, WI, United States

P. Galen DiDomizio, MD (he/him/his)
Assistant Professor of Pediatrics
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Both complex care and palliative care programs accept clinical responsibility of children with medical complexity (CMC). There is sparse data investigating best practices for collaboration between the two programs in caring for this shared population.
Objective: The aims of this study were to explore the distinct and overlapping roles of complex care and palliative care programs when caring for CMC, as well as to identify the facilitators and barriers to their collaboration.
Design/Methods: We conducted a qualitative study using semi-structured interviews. Eligible participants were pediatric physicians or advanced practice providers practicing complex care or palliative care at academic medical centers within the Midwestern United States. Data obtained from interviews were audio-recorded, transcribed, coded, and analyzed by two independent reviewers using thematic analysis.
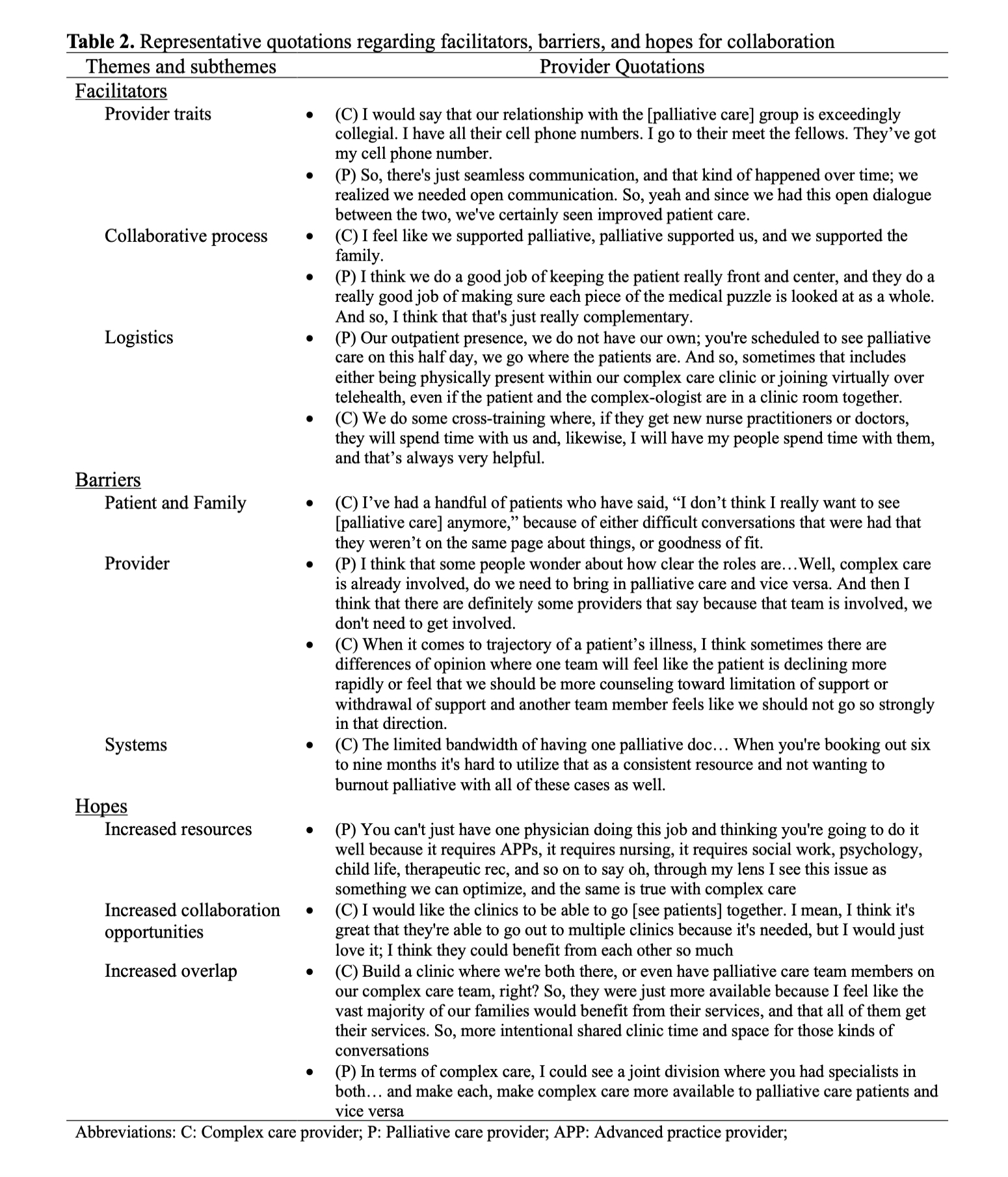
Results: 18 providers (8 complex care and 10 palliative care) across 10 centers completed semi-structured interviews. Interviews revealed that both programs operate within a spectrum of clinical roles, thematically organized as complex-leaning, palliative-leaning, or blended (Table 1). Program roles were more often defined by the unique provider-family relationships rather than by clear boundaries between the two programs. Regarding program collaboration, facilitator subthemes included provider traits, collaborative process, and logistics. Providers identified family, provider, and systems-based barrier subthemes. Providers expressed hope for improved future collaboration through increased resources, increased collaboration opportunities, and increased overlap between programs, including shared staff or divisions (Table 2).
Conclusion(s): Pediatric complex and palliative care programs often overlap when caring for CMC, which can potentially lead to duplication or fragmentation of care. This study demonstrated that although many barriers to collaboration exist, providers across institutions have identified potential avenues to improve partnerships across disciplines. Future research should aim to capture patient and caregiver perspectives when utilizing both teams concurrently. This study will inform the development of best practices and subsequent design of interventions to integrate disparate teams when caring for CMC.
Table 1. Representative quotations regarding spectrum of clinical roles
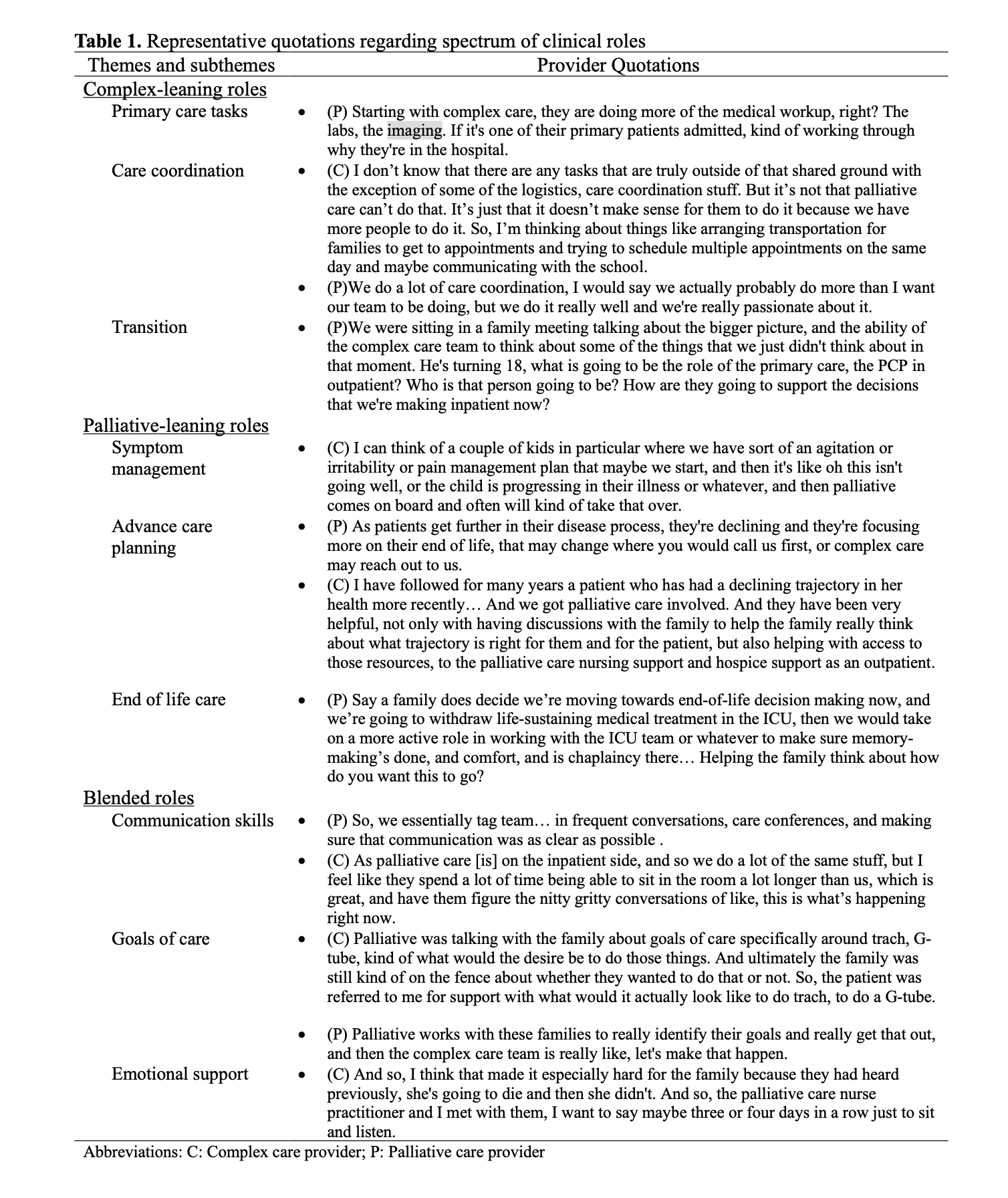
Table 2. Representative quotations regarding facilitators, barriers, and hopes for collaboration
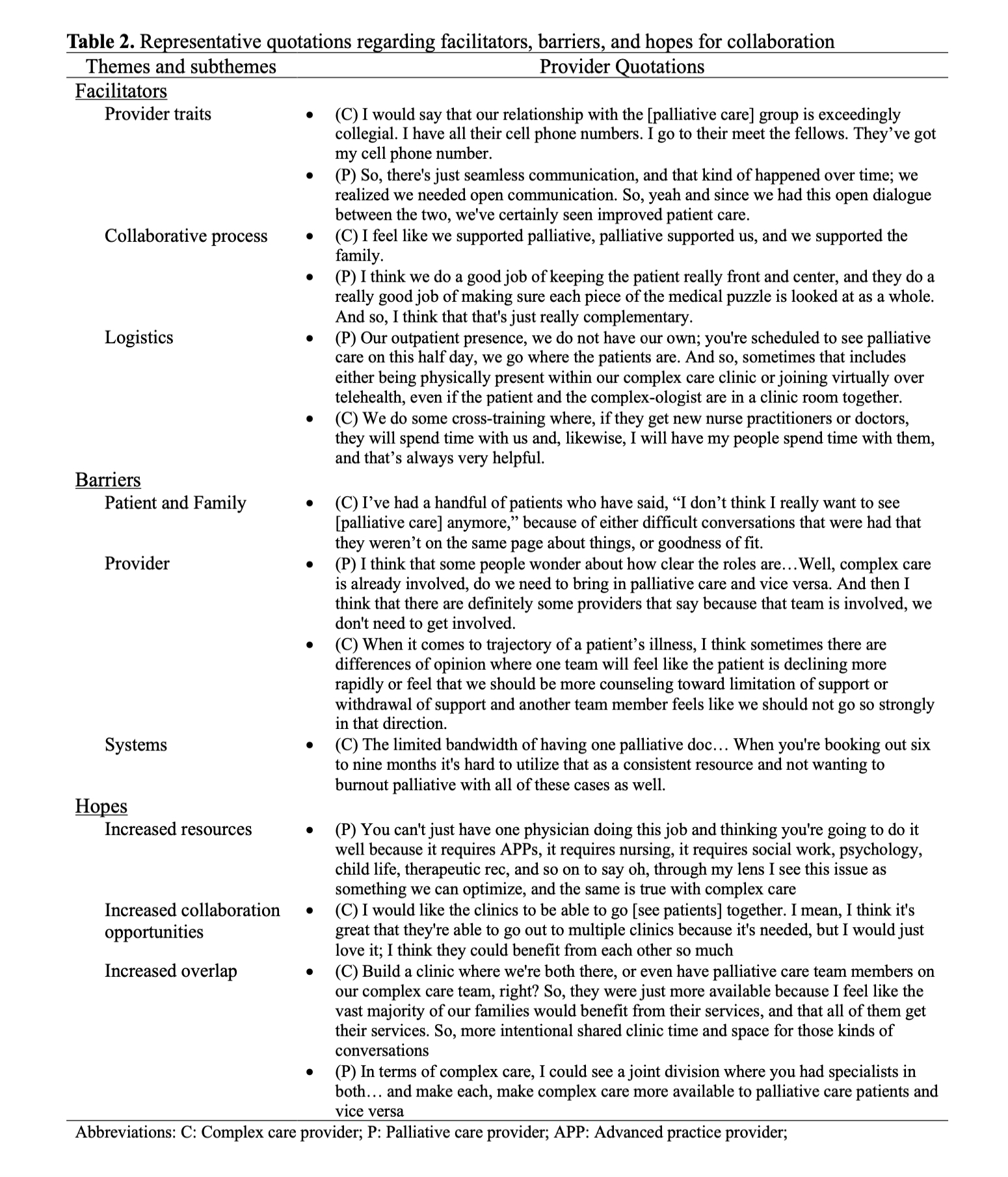
Table 1. Representative quotations regarding spectrum of clinical roles
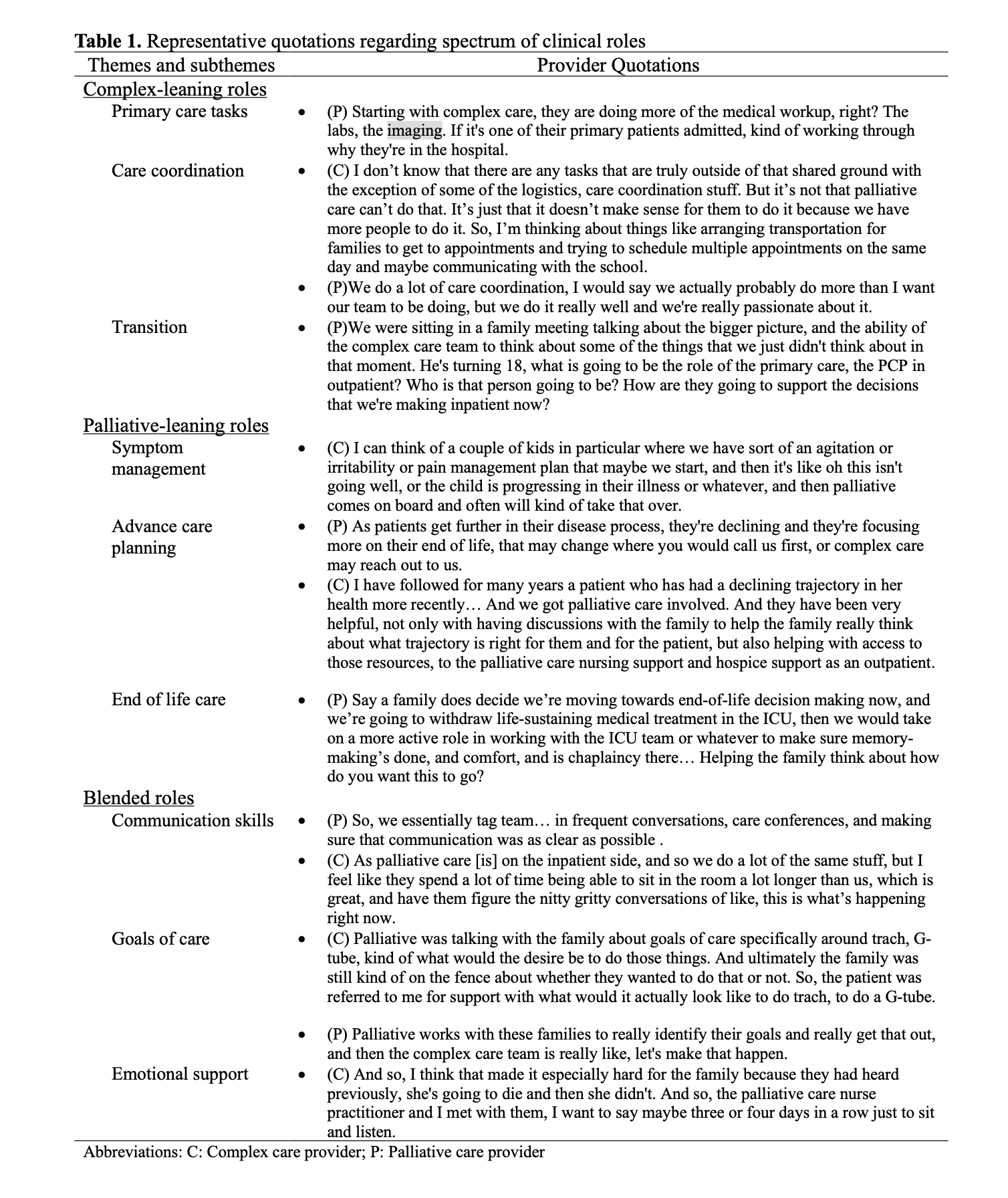
Table 2. Representative quotations regarding facilitators, barriers, and hopes for collaboration