Critical Care 2
Session: Critical Care 2
128 - Sleep disturbances after hospitalization in children with traumatic brain injury
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 128.6894
Cydni Williams, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Trevor Hall, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States

Cydni Williams, MD, MCR (she/her/hers)
Associate Professor of Pediatrics
Doernbecher Children's Hospital at Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Traumatic brain injury (TBI) is a leading cause of disability in children. Survivors of TBI face long-term physical, cognitive, and psychosocial morbidities. Sleep is critical to brain health and repair after injury; however, TBI survivors commonly have problems with initiation and maintenance of sleep.
Objective: We aimed to determine the prevalence of disturbances in initiation and maintenance of sleep after hospitalization in children with TBI and evaluate associations between measures of sleep and physical, cognitive, and psychosocial health. We hypothesized sleep disturbances would be associated with worse outcomes at 6-months following discharge.
Design/Methods: We conducted a prospective cohort study of children aged 6 – 18 years of age hospitalized with TBI and followed over 6-months (N=54, Table 1). Sleep initiation and maintenance were evaluated using the Sleep Disturbances Scale for Children Disorders of Initiation and Maintenance of Sleep Scale (DIMS) and wrist actigraphy measuring sleep times, onset latency, and efficiency. Scores were compared to historical healthy controls using independent t-tests. Health outcomes included questionnaires for executive function, quality of life, fatigue, anxiety, depression, and pain. Relationships between sleep and outcome measures were evaluated using Spearman correlation (r). Significance defined as p<.05.
Results: Clinically significant concerns (DIMS T-score ≥60) were found in in 63% at 3-months and 59% at 6-months. Compared to their reported baseline, 29% of the cohort at 3-months and 40% at 6-months had an increase of ≥1 standard deviation (SD) in the DIMS T-score. Similarly, actigraphy measures at 3 and 6-months showed significantly longer sleep onset latency and reduced sleep efficiency when compared to healthy historical controls (Table 2). No significant associations were found between DIMS T-score and demographic or clinical characteristics, while older age was associated with longer latency and lower efficiency on actigraphy at both timepoints. Significant correlations were found between DIMS and measures of executive function, quality of life, fatigue, anxiety, depression, and pain 6-months after TBI (Figure 1). Similarly, both longer onset latency and lower sleep efficiency significantly correlated with fatigue and depression (r=.45-.53, p<.05).
Conclusion(s): Clinically significant sleep disturbances are common in children after TBI hospitalization. Difficulty with sleep onset and maintenance correlate with worse physical, cognitive, and psychosocial health 6-months after TBI.
Table 1. Cohort demographic and clinical characteristics
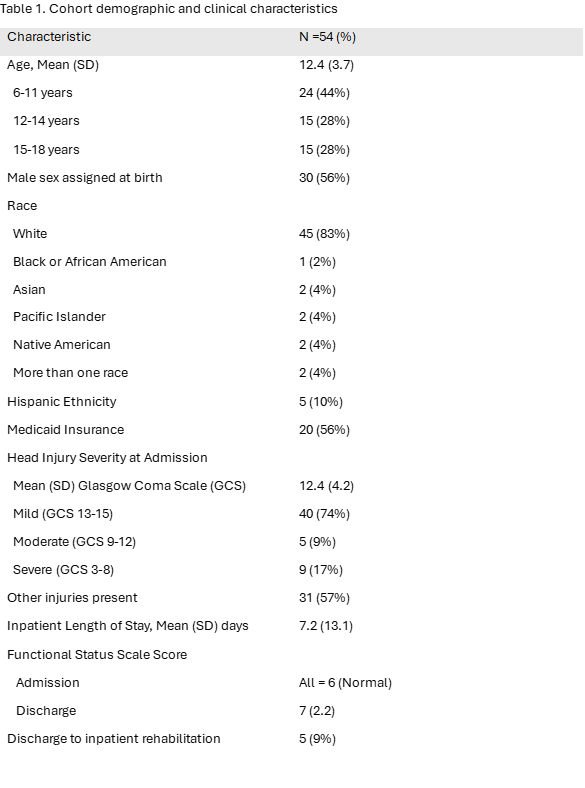
Table 2. Comparison of traumatic brain injury cohort scores on wrist actigraphy to reference values in healthy pediatric cohorts

Figure 1.
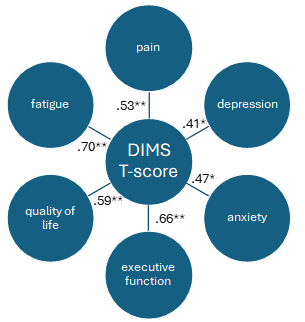 Spearman Correlations (r) between Sleep Disturbances Scale for Children Disorders of Initiation and Maintenance of Sleep (DIMS) scale and health outcomes 6-months after traumatic brain injury. *p <.05, **p <.01
Spearman Correlations (r) between Sleep Disturbances Scale for Children Disorders of Initiation and Maintenance of Sleep (DIMS) scale and health outcomes 6-months after traumatic brain injury. *p <.05, **p <.01
