Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
062 - Structured Handoff Initiative for Facilitating Transitions (S.H.I.F.T.) in the NICU
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 62.6884
Lucy A.. Rubin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Cameron N.. Boyd, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Imran M. Ilahi, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; John E.. Mascari, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Spencer M. Millen, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Justyna Grothaus, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
- LR
Lucy A. Rubin, MD
NICU Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Provider handoffs in the NICU present a major opportunity for error and patient harm, especially for complex infants in level IV care. Miscommunication during these transitions can lead to serious adverse events.
Objective: To design and implement a standardized handoff process in a level IV NICU that improves the efficiency and accuracy of daily sign-out.
Design/Methods: A pre-intervention survey was distributed to faculty and fellows. Using Epic, a standardized sign-out was created with key clinical information for each patient. Daytime teams were asked to sign-out patients with high acuity, difficult airways, DNR/DNI status, and anyone else they have concerns about. Non-critical patient calls were deferred until after sign-out. Daily sign-out was observed on 20 weekdays, with documentation of duration, interruptions, and instances of teaching. Throughout the study period, a brief survey was distributed to the post-call team to determine if the sign-out they received was accurate and adequate. Post-intervention, daily sign-out was again observed on 20 weekdays and a post-intervention survey was distributed.
Results: -Pre-intervention Survey: 80% response rate. The most significant perceived barriers to effective sign-out were: duration, irrelevant information, and number of interruptions.
-Process Metrics (utilizing a standardized EMR sign-out available in Epic): Sign-outs were distributed to on-call faculty before sign-out.
-Outcome Metrics (length of sign-out and number of interruptions): Pre-intervention, sign-out took an average of 72 minutes with at least 1 interruption 70% of the time. Post-intervention, sign-out took an average of 42.7 minutes with at least 1 interruption 25 % of the time. The run charts are depicted in Figures 1 and 2. The control chart (Figure 3) shows time spent per patient (1.3 minutes pre-intervention and 0.78 minutes post-intervention, a statistically significant decrease).
-Post- intervention survey: 80% response rate. The majority (79%) of respondents want to continue using the new sign-out format.
-Balancing metrics (sign-out accuracy and fellow teaching occurrences): Post-call surveys showed that providers received all pertinent information needed for overnight care 100% of the time (pre-intervention) and 94% of the time (post-intervention). The frequency of fellow teaching did not decrease during our observation period.
Conclusion(s): The implementation of a standardized and abbreviated sign-out utilizing the EMR in a level IV NICU saved valuable clinician time and minimized interruptions, without sacrificing accuracy of sign-out or learning opportunities for fellows.
Figure 1. Run chart of total duration of sign-out (in minutes)
.png)
Figure 2. Run chart of number of interruptions during sign-out
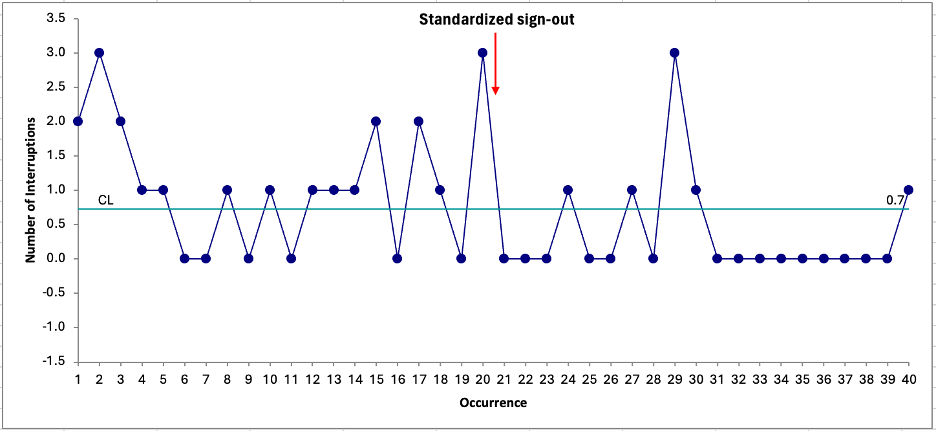
Figure 3. Control chart of sign-out time per patient (in minutes)
.png)


