Cardiology 2
Session: Cardiology 2
158 - Socioeconomic influences on Prenatal Detection of Critical Congenital Heart Disease during the COVID pandemic
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 158.6832
Alejandra Mallorga Hernandez, Children's Hospital Los Angeles, Los Angeles, CA, United States; Shuo Wang, Children's Hospital Los Angeles, Los Angeles, CA, United States; Jay Pruetz, Children's Hospital Los Angeles, Culver City, CA, United States

Alejandra Mallorga Hernandez, MD, MPH (she/her/hers)
Resident physician
Children's Hospital Los Angeles
Los Angeles, California, United States
Presenting Author(s)
Background: Prenatal diagnosis (PD) of critical congenital heart disease (CCHD) has increased over time with advancements in imaging technology, improved fetal echocardiography (FE) guidelines and more training opportunities. The COVID pandemic amplified health care disparities including factors influencing rates of PD.
Objective: This study sought to clarify the role that socioeconomic status (SES) and demographic factors had on PD rates of CCHD during the COVID pandemic.
Design/Methods: This was a single center retrospective study of newborns with CCHD admitted to our institution for cardiac intervention (n=209) during the pandemic period (03/2020 to 03/2022). Based on previously validated measures by the Robert Graham center using data from the 2020 US Census, social deprivation index (SDI) scores were calculated for each patient based on their zip code tabulation areas to assess SES. ArcGIS was used to map SDI for the patient population included in our study, which was divided in quartiles for analysis (Fig 1). Univariate and multivariate analysis were used to evaluate the relationship between PD and SDI, lesion type (single ventricle vs outflow tract anomalies vs other lesions, comprised of historically harder to detect lesions in utero), race, maternal age, and insurance type.
Results: Each patient’s cardiac diagnosis was classified by FE findings into the following mutually exclusive groups: (1) single ventricle variants (n=50); (2) outflow tract (OFT) anomalies (n=91); and (3) other lesions (n=68), comprised mostly of aortic arch obstruction anomalies (n=52). PD occurred in 144 patients (68%). On univariate analysis private insurance and maternal age (>35yo) were significantly associated with higher PD rate (p=0.014 and p=0.037 respectively) while race, ethnicity and English proficiency were not associated with PD (Table 1). On multivariate analysis, SES patients across all quartiles had comparable PD rates for Group 1, single ventricle, and Group 2, OFT anomalies. However, higher SES patients were 7 times more likely to have a PD in Group 3, lesions with historically lower detection rates in utero (odds ratio 7.04, 95% CI, 1.6 to 31.2, p=0.0106).
Conclusion(s): Private insurance and maternal age >35years were independently associated with increased PD of CCHD during the COVID pandemic. PD of single ventricle and OFT lesions were not significantly affected by SES. However, higher SES was associated with increased PD of lesions historically harder to diagnosis in utero.
Figure 1. Social Deprivation Index (SDI) for patient population in study
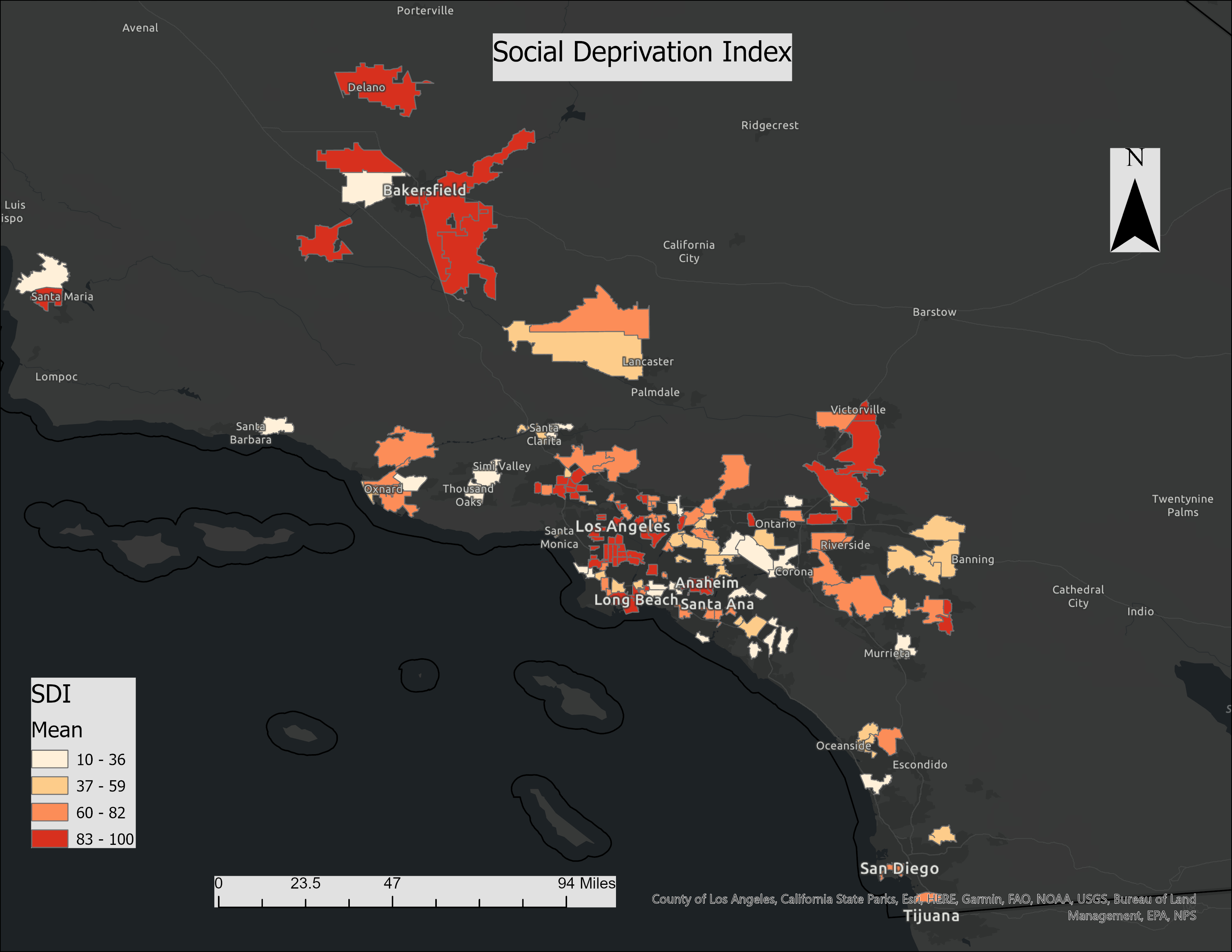 SDI is the composite measure of area level deprivation based on census data used to quantify the socio-economic variation in health outcomes. As the SDI score increases (darker shades), the severity of deprivation increases. In this figure, ArcGIS was used to map SDI for the patient population included in our study.
SDI is the composite measure of area level deprivation based on census data used to quantify the socio-economic variation in health outcomes. As the SDI score increases (darker shades), the severity of deprivation increases. In this figure, ArcGIS was used to map SDI for the patient population included in our study. Table 1. Comparison of patients with and without prenatal diagnosis (PD) by patient characteristics (univariate analysis).
.png) On the univariate analysis, CCHD category, maternal age, and insurance type were noted to have a significant effect on prenatal diagnosis of CCHD during the COVID pandemic. SDI impact on PD for all lesions as a singular group, was noted to be non-significant. However, on further multivariate analysis, it was found that while SDI did not play a key role for PD of single ventricle and OFT lesions, it significantly impacted PD for Group 3, lesions with historically lower detection rates in utero. In this group, infants with higher SES were 7 times more likely to be diagnosed prenatally (odds ratio 7.04, 95% CI, 1.6 to 31.2, p=0.0106).
On the univariate analysis, CCHD category, maternal age, and insurance type were noted to have a significant effect on prenatal diagnosis of CCHD during the COVID pandemic. SDI impact on PD for all lesions as a singular group, was noted to be non-significant. However, on further multivariate analysis, it was found that while SDI did not play a key role for PD of single ventricle and OFT lesions, it significantly impacted PD for Group 3, lesions with historically lower detection rates in utero. In this group, infants with higher SES were 7 times more likely to be diagnosed prenatally (odds ratio 7.04, 95% CI, 1.6 to 31.2, p=0.0106).
