Emergency Medicine 2
Session: Emergency Medicine 2
432 - Testicular Ultrasound Use in Pediatric EDs: Trends, Age-Related Findings, and Predictors of Testicular Torsion
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 432.6812
Patrick S. Walsh, Medical College of Wisconsin, Milwaukee, WI, United States; Patrick Drayna, Medical College of Wisconsin, Cedarburg, WI, United States; Amanda S. Dupont, Medical College of Wisconsin, Mequon, WI, United States; Jonathan Ellison, Medical College of Wisconsin, Milwaukee, WI, United States; Kevin P. Boyd, Medical College of Wisconsin, Milwaukee, WI, United States; sri Chinta, Medical College of Wisconsin, Milwaukee, WI, United States

Patrick S. Walsh, MD, MS
Assistant Professor
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Acute scrotal pain is a common presenting symptom in the pediatric emergency department (ED). Ultrasound is commonly used in conjunction with clinical findings to evaluate for testicular torsion, a surgical emergency. Patterns of use of scrotal ultrasound, as well as the common diagnoses found when ultrasounds are performed, have not been well described.
Objective: To characterize the use of scrotal ultrasound in tertiary pediatric EDs and to determine the frequency of testicular torsion and other diagnoses.
Design/Methods: This was a retrospective cross-sectional study of 38 hospitals in the Pediatric Health Information System database. We included ED encounters from 2016-2023 that involved a scrotal or testicular ultrasound. We summarized the number of ED visits with testicular ultrasounds each year and patterns over time. We described the ICD-10 diagnoses associated with these encounters, including testicular torsion, torsion of the appendix testis, epididymitis/orchitis, hydrocele, hernia, varicocele, and epididymal cyst. We used mixed effects logistic regression to assess associations of age, race and ethnicity, and insurance status with a diagnosis of testicular torsion, adjusting for clustering by hospital.
Results: There were 120,350 ED encounters with a scrotal ultrasound during the study period. The median age was 10 (IQR: 5-13) years. The cohort was 46% Non-Hispanic White, 15% Non-Hispanic Black, and 27% Hispanic. Scrotal ultrasound use increased each year except in 2020 (Figure 1). Testicular torsion was diagnosed in 7.3% of encounters but was more common in children over 11 years (14%) than those age 10 and under ( < 3%). For non-torsion diagnoses, hydroceles were diagnosed in 41% of encounters for children under 2 years while epididymitis/orchitis was diagnosed in 21% of children aged 6-10 years (Figure 2). In multivariable analysis, children aged 11+ had significantly higher odds of testicular torsion (OR: 6.41; 95% CI: 5.78-7.11) compared to those under 2 years, and Non-Hispanic Black children had higher odds of torsion (OR: 1.96; 95% CI: 1.84-2.10) compared to Non-Hispanic White children. (Table 1).
Conclusion(s): Scrotal ultrasound use increased over time in pediatric EDs. Age and race were associated with variation in diagnoses, with older age and Non-Hispanic Black race linked to higher odds of testicular torsion. These findings raise questions about the factors driving variation in use of scrotal ultrasound across different patient groups and may inform strategies to optimize its utility.
Figure 1: Testicular Ultrasound Use Over Time
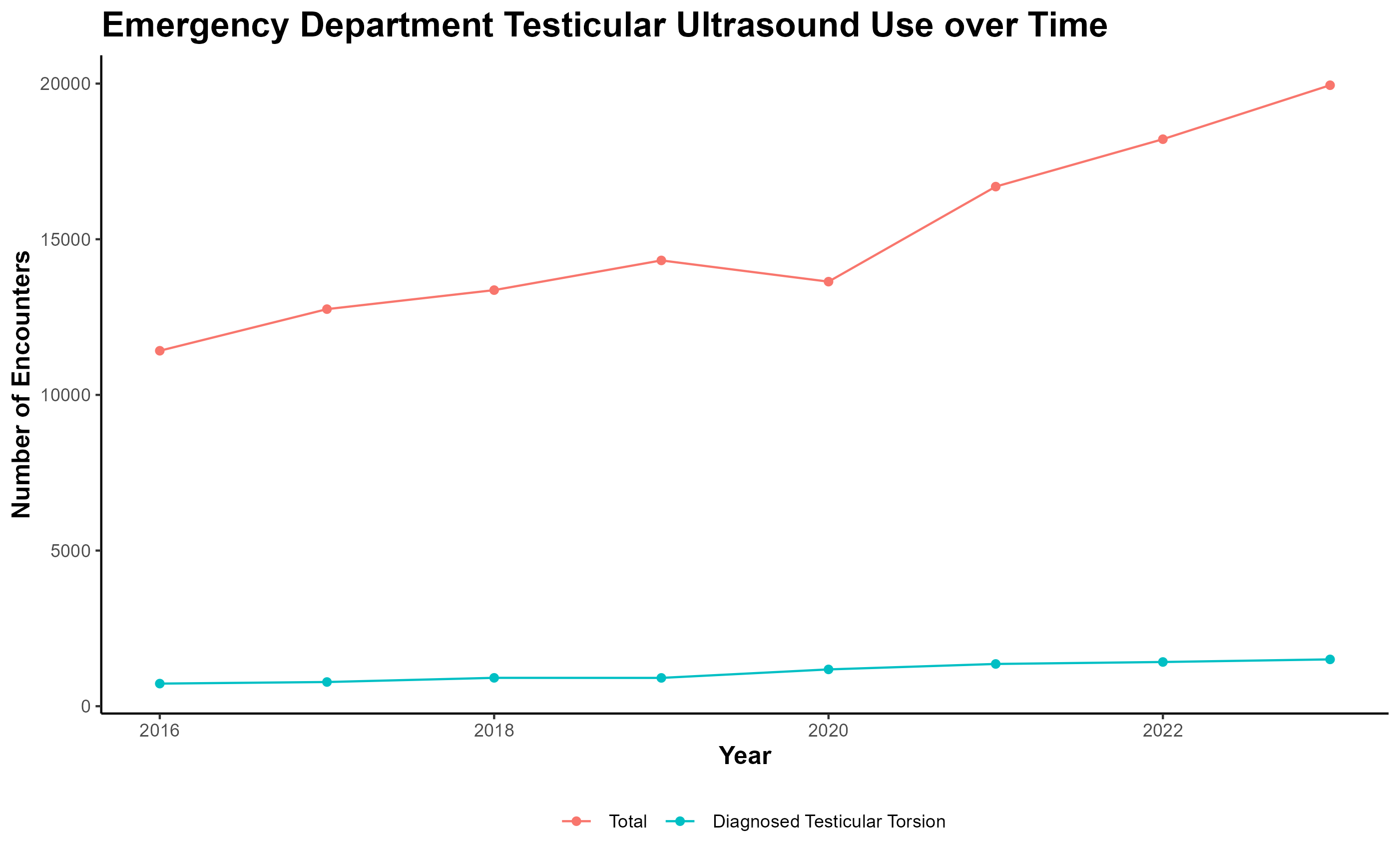 Number of ED encounters with a testicular ultrasound at 38 pediatric hospitals each year from 2016-2023. Red: all ultrasound encounters; Blue: encounters with an associated diagnosis of testicular torsion.
Number of ED encounters with a testicular ultrasound at 38 pediatric hospitals each year from 2016-2023. Red: all ultrasound encounters; Blue: encounters with an associated diagnosis of testicular torsion.Figure 2: Diagnoses Associated with Emergency Department Visits with Testicular Ultrasound
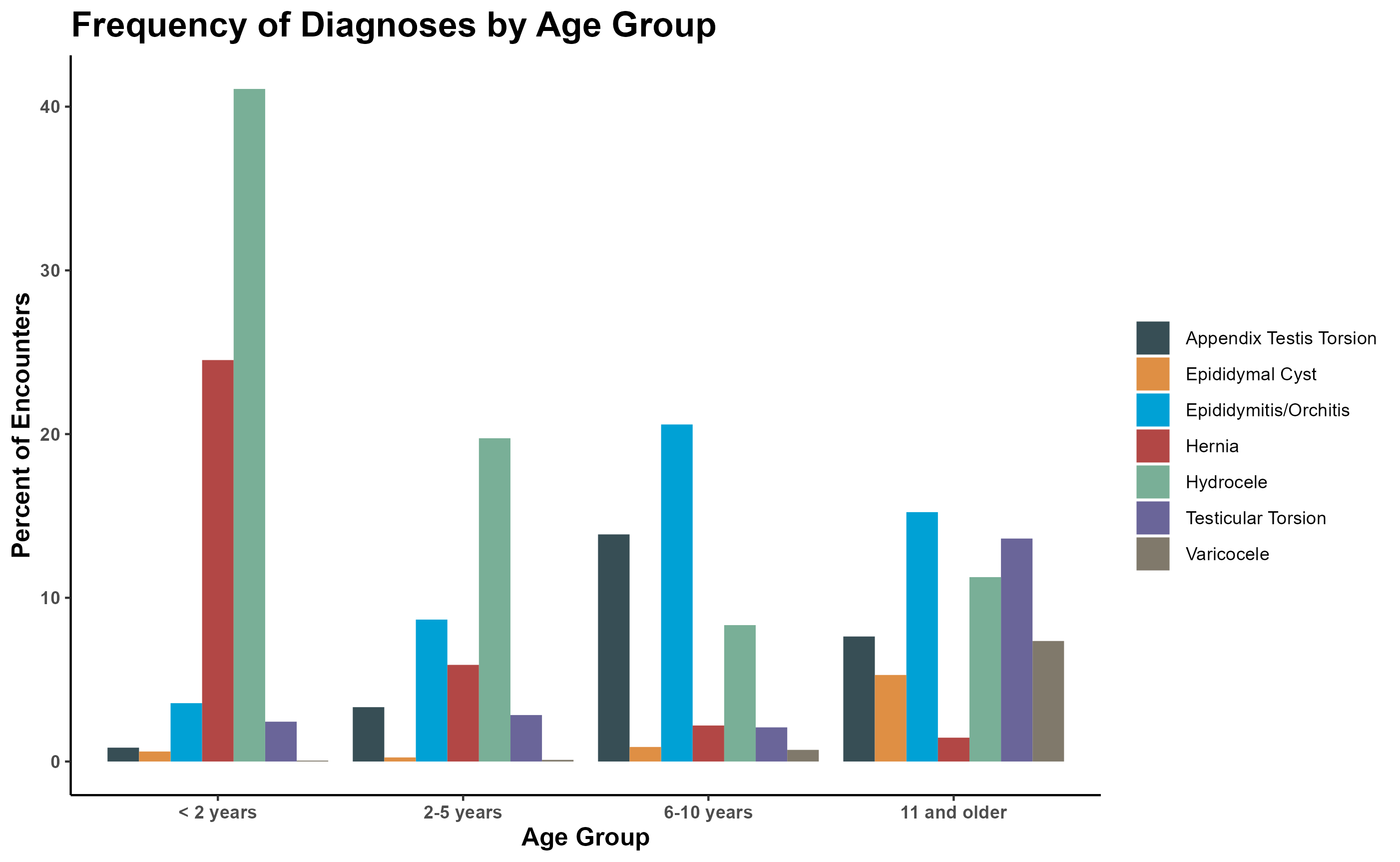 This figure demonstrates the proportion of ultrasound encounters in each age group with different diagnoses.
This figure demonstrates the proportion of ultrasound encounters in each age group with different diagnoses. Table 1: Association of Demographic Factors with Testicular Torsion Diagnosis
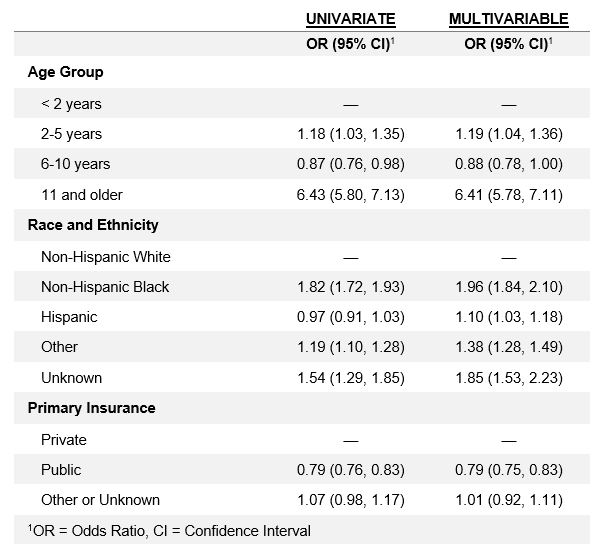 Results from mixed-effects logistic regression models adjusting for clustering by hospital.
Results from mixed-effects logistic regression models adjusting for clustering by hospital.
