Emergency Medicine 2
Session: Emergency Medicine 2
434 - The Lived Experience of Completing the National Pediatric Readiness Project (NPRP) Assessment: The Case for a Multidisciplinary, Team-based Approach
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 434.6808
Jennifer Jamerino-Thrush, Children's Hospital of Michigan, West Bloomfield, MI, United States; Catie Guarnaccia, University of Michigan Medical School, Ypsilanti, MI, United States; Samantha Kesterson, University of Michigan Medical School, Ann Arbor, MI, United States; Michelle Macy, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Courtney W.. Mangus, C.S. Mott Children's Hospital, Ann Arbor, MI, United States; Megan Norris, Michigan Emergency Department Improvement Collaborative, Ann Arbor, MI, United States; Michele Nypaver, University of Michigan Medical School, Ann Arbor, MI, United States; Emily Mathias, University of Michigan Medical School, Ann Arbor, MI, United States

Jennifer Jamerino-Thrush, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Hospital of Michigan
West Bloomfield, Michigan, United States
Presenting Author(s)
Background: The NPRP provides emergency departments (ED) with a free, web-based assessment to gauge their ability to care for ill and injured children. Results of this self assessment inform quality improvement (QI) initiatives aimed at improving pediatric emergency care at local, state and national levels. In 2021, the NPRP conducted a national assessment, providing a comprehensive snapshot of pediatric readiness in >70% of EDs across the United States. The process and overall experience of completing the assessment at the local ED level has not previously been studied.
Objective: 1) To gain real-time insight on the experience of completing the NPRP assessment in community EDs.
2) To identify opportunities to better support successful NPRP assessment completion in the future.
Design/Methods: As part of an ongoing QI initiative led by the Michigan Emergency Department Improvement Collaborative (MEDIC), in-person, on-site, observed assessment events were conducted with each of the 6 participating community EDs. Prior to the assessment, event sites were asked to review assessment questions and identify key informants, their “pediatric readiness team”, to be present or contribute to assessment completion. During the events, teams completed the online assessment by answering questions to the best of the team’s ability through consensus. When applicable, supporting documents and equipment were verified. Concurrently, MEDIC team members recorded observations during the completion process. After assessment completion, the team participated in an audio recorded debriefing session facilitated by MEDIC. Qualitative content analysis of debriefing session transcripts was utilized with descriptive coding proceeded by consensus between at least two coders. Key themes were developed and refined through discussion.
Results: Six general hospital EDs completed an assessment event. Key informant roles identified by every site included ED nurse manager, ED physician and trauma program manager. The ED pharmacist, although not consistently identified, was noted to be valuable for assessment completion and follow-up. The assessment question on competency requirements was most difficult to answer. Emerging themes include multidisciplinary involvement to optimize assessment accuracy, desire for clarification on assessment questions, and the emerging role of the trauma team in ED pediatric readiness.
Conclusion(s): Completing the pediatric readiness assessment as a multidisciplinary team facilitated increased confidence in the accuracy of responses, established the importance of concerted QI efforts, and provided space to determine action steps.
Enrolled Sites - Descriptive Data
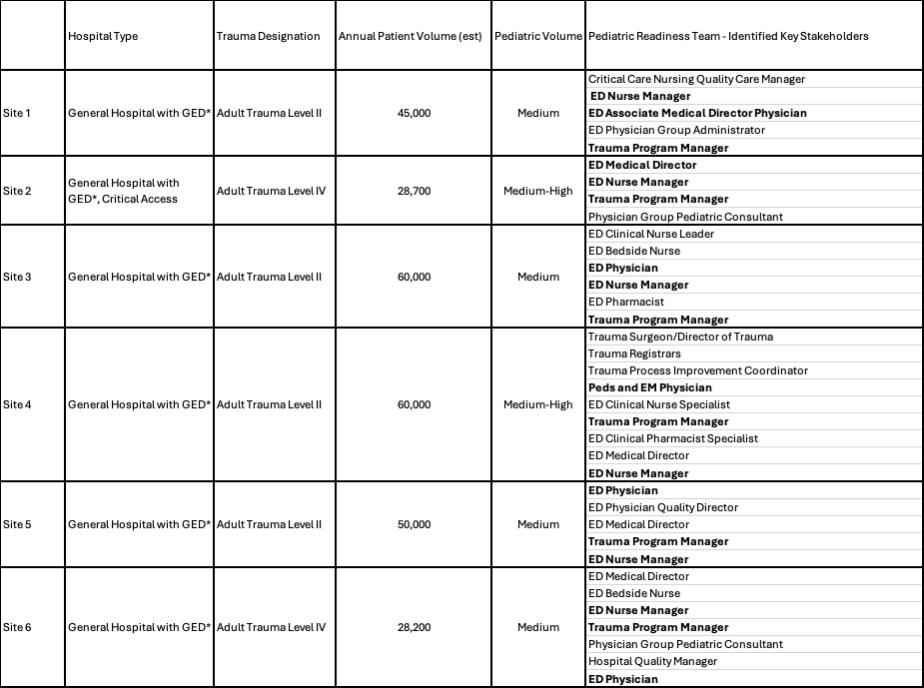 Descriptive data for enrolled hospital sites. *GED = general emergency department. Text in bold indicates key informant roles identified by each of the 6 sites.
Descriptive data for enrolled hospital sites. *GED = general emergency department. Text in bold indicates key informant roles identified by each of the 6 sites.Debrief Transcripts Emerging Themes with Example Quotes
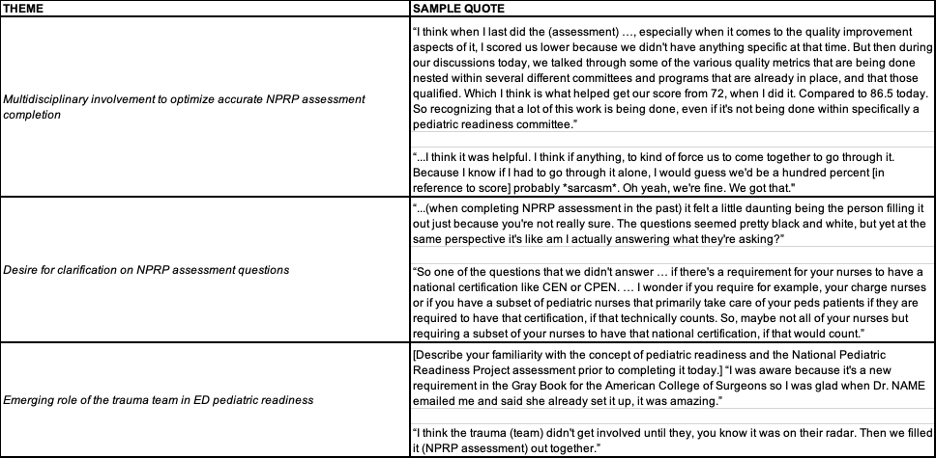 Various emerging themes from debrief transcripts with example quotes.
Various emerging themes from debrief transcripts with example quotes. 
