Emergency Medicine 2
Session: Emergency Medicine 2
433 - The Building Blocks of Pediatric Readiness: Using Organizational Hierarchy to Identify Targets for Collaborative Improvement of National Pediatric Readiness Project Scores at a Large Public Hospital
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 433.6939
Alexandra K.. Monroe, Emory University School of Medicine, Atlanta, GA, United States; Carey K.. Lamphier, Grady, Atlanta, GA, United States; Laura S. Johnson, Emory University School of Medicine, Atlanta, GA, United States; S. Rob Todd, Grady Memorial Hospital, Atlanta, GA, United States; Pamela W. Vanderberg, Grady Memorial Hospital, Atlanta, GA, United States; Daniel Wu, Emory University School of Medicine, Atlanta, GA, United States; Elizabeth Benjamin, Emory University School of Medicine, Atlanta, GA, United States

Alexandra K. Monroe, MD, MPH (she/her/hers)
Assistant Professor
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
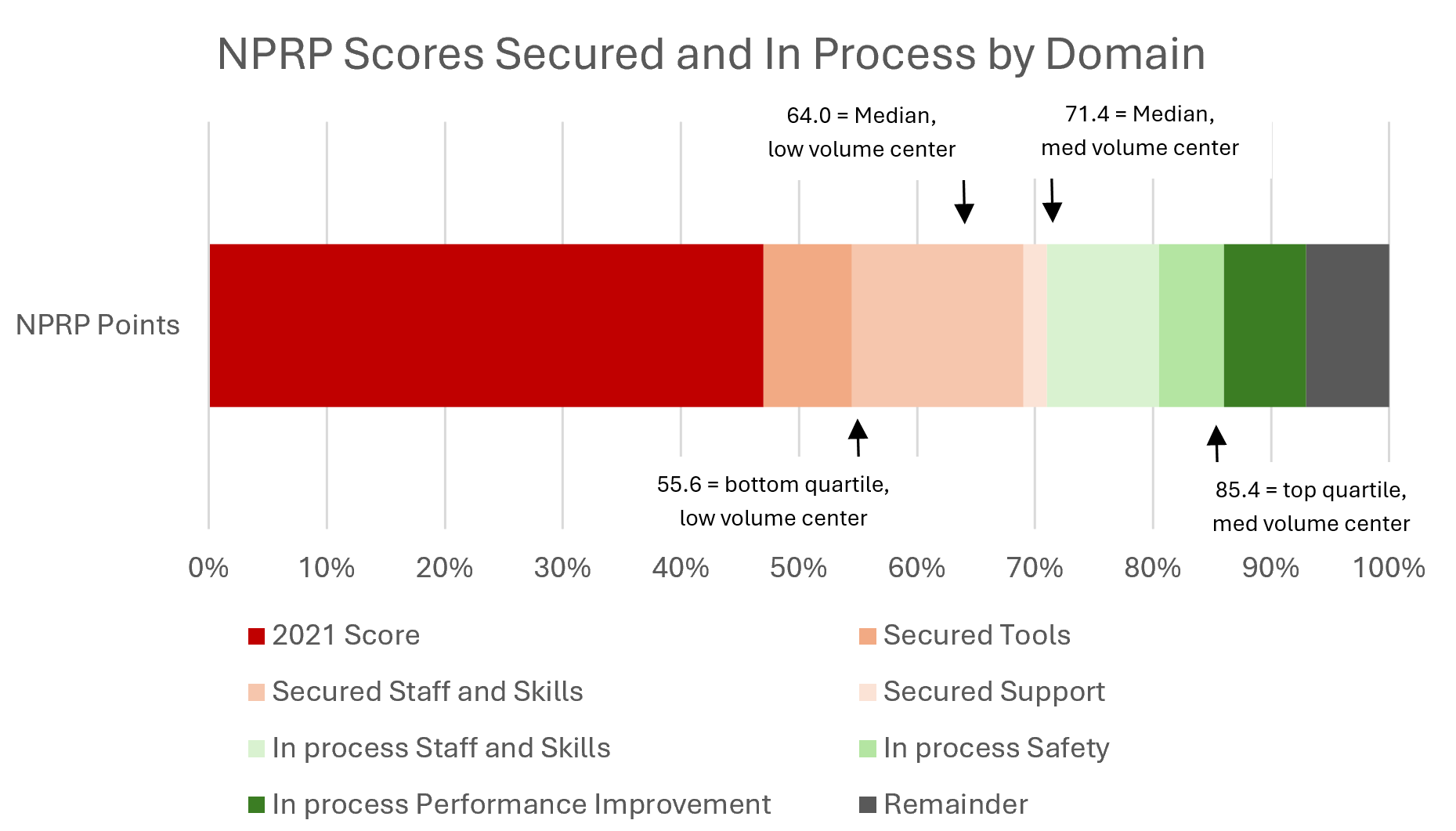
Background: Our hospital is one of the largest public hospitals in the US and interfaces with pediatric patients in flagship programs like emergency care, trauma, and burn without a mechanism to evaluate our pediatric scope or effectiveness. This is reflected in our 2021 National Pediatric Readiness Project (NPRP) score of 47, which falls in the lowest quartile.1 As children's hospital capacity narrows nationwide, pediatric care at safety net hospitals increases and is reflected in our pediatric ED volume trends (Figure 1).
Objective: To address our pediatric readiness challenges, collaborators in the Departments of Pediatrics, Emergency Medicine, Surgery, and Nursing Administration applied NPRP concepts to a hospital-wide quality improvement effort.
Design/Methods: Stakeholders performed key driver and value analyses of our NPRP Score and Gap Analysis. Identified targets were arranged based on the organizational hierarchy of needs to determine highest priority (Figure 2).
Supplies: Standardized Broselow cart through central supply chain management and checkoff procedures
Staff and Skills: Secured one shift/week of protected time for RN-PECC and invested in nationally recognized PALS and ENPC courses
Safety: Identified discrepancies between safety policies and case review; developed “code sheets” with precalculated medication doses based on estimated weight and formulary
Support: Identified policies, procedures, and protocols needing updates and included pediatric patients in disaster management plan, mutual aid agreements, and MCI drills
Performance Improvement: Developing a pediatric registry informing our performance improvement plan with patient data and quality metrics; proposed a Pediatric Oversight Committee to centralize subject matter expertise, increase standardization, and pool resources
Results: Our NPRP score improved from 47 to an ~71 with our interventions. This is a 51% improvement in score, but is still below the median for our new status as a medium volume center based on ED volume trends. Continued investment could secure 22 more points, totaling 93. This would be ~100% improvement and place us in the top quartile for medium volume centers1,2 (Figure 3).
Conclusion(s): We utilized an organizational hierarchy of needs to identify sustainable solutions for our NPRP Gap Analysis. Despite our success, implementation challenges include discrepancies between policy and daily practice, highlighting the need for continuous evaluation of NPRP metrics by a pediatric oversight committee co-lead by both an MD and RN PECC. Ongoing NPRP investment could propel us to become a leader among our peer group hospitals.
Figure 1. Number of Emergency Department Encounters by Age in Years Range
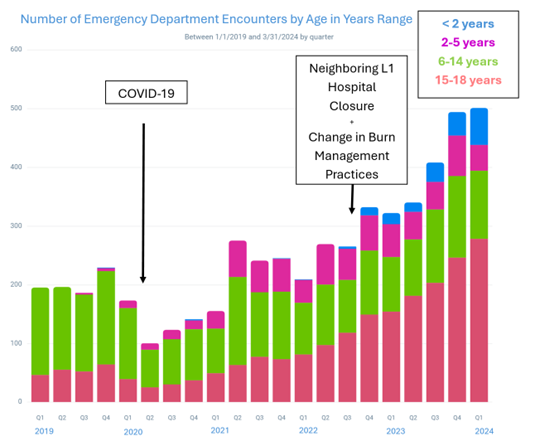
Figure 2. Organizational Hierarchy of Needs for NPRP Key Drivers
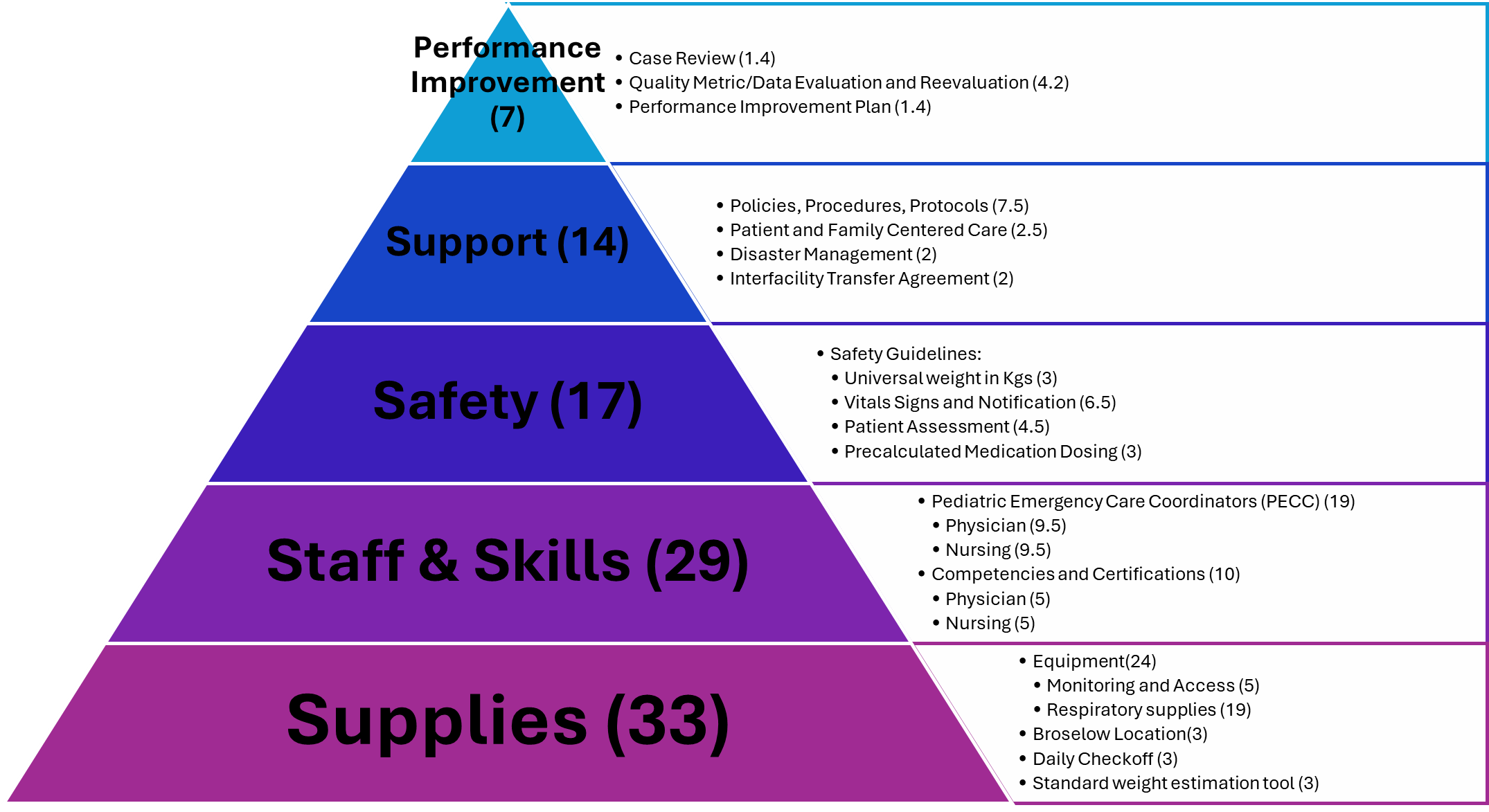
Figure 3. NPRP Scores "Secured" and "In Process" by Domain