Emergency Medicine 3
Session: Emergency Medicine 3
445 - Risk of Invasive Bacterial Infection in Febrile Infants with Concurrent UTI: A Subgroup Analysis by Age
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 445.6280
Jacob Phouthavong-Murphy, Phoenix Children's Hospital, Tempe, AZ, United States; Jared Kusma, Phoenix Children's, Phoenix, AZ, United States; Quinney Fu, Phoenix Children's, Phoenix, AZ, United States; Maheshwor Kafle, Phoenix children’s hospital, Phoenix, AZ, United States; Jennifer Stamp, Phoenix Children's Hospital, Phoenix, AZ, United States; Ashley Bartlett, Phoenix Children's Hospital, Scottsdale, AZ, United States; Richard Engel, Phoenix Children's Hospital, Phoenix, AZ, United States; Jillian Wall, Phoenix Children's Hospital, Phoenix, AZ, United States; Sandra Gage, Phoenix Children's Hospital, Racine, WI, United States

Jacob Phouthavong-Murphy, DO (he/him/his)
Pediatric Resident
Phoenix Children's Hospital
Tempe, Arizona, United States
Presenting Author(s)
Background: Unidentified invasive bacterial infection (IBI) in febrile infants can have severe consequences. The AAP 2021 febrile infant clinical practice guideline (CPG) provides clear recommendations to obtain cultures and inflammatory markers for risk stratifying based on age (8-21, 22-28, and 29-60 days-old [DO]). The recommendations change with age due to the significant increase in identified bacteremia in the younger age group. Of note, the CPG's recommendation for further work-up with a concerning urinalysis differs based on age.
Objective: (1) Assess the risk of IBI in febrile infants within age groups for those with and without UTI. (2) Assess the risk of IBI in febrile infants with UTI between age groups.
Design/Methods: This IRB-approved single tertiary center retrospective cohort study examined febrile infants 8-60 DO who presented between 01/01/2018-12/31/2023. Patients were identified using ICD-10 codes for fever or bacterial infection. Exclusion criteria: prematurity ( < 37 weeks), prior ICU admission, previous antibiotic administration, complex care needs, focal source of infection without cultures, and infants with missing blood or urine cultures. Data collected: age, blood/CSF/urine culture, and urinalysis. To be considered UTI+, urine culture growth must be accompanied by urinary white blood cells (WBC) ≥3 cells/HPF, positive leukocyte esterase, or positive nitrites. Relative risk (RR) was calculated with statistical significance compared using 95% confidence intervals (CI).
Results: A total of 2073 infants met inclusion criteria; details of IBI and UTI occurrence noted in Table 1. The overall RR for IBI with concurrent UTI was 8.13. Relative risk of IBI in UTI+ vs UTI- infants aged 8-21, 22-28, and 29-60 DO were 5.85, 1.46 and 9.24, respectively (Table 2). A pairwise comparison found UTI+ infants aged 8-21 DO have a higher risk of IBI compared to both infants aged 22-28 and 29-60 DO (7.59 and 2.24, respectively; Table 3). There was no change in relative risk of IBI in UTI+ when comparing 22-28 and 29-60 DO (Table 3).
Conclusion(s): Compared to 8-21 DO infants, 29-60 DO infants appear to have a higher RR of IBI when UTI is present, likely due to the lower percentage of IBI in the older patient population magnifying the impact UTI has on their risk. When comparing UTI+ infants across age groups, the youngest infants showed a significantly higher risk of IBI than both older groups supporting the AAP guidelines that stratify recommendations based on age. Clinicians should consider the elevated risk of IBI when UTI is present, especially in febrile infants under 22 DO.
Table 1: Distribution of included patients based on age and infection status with rate of IBI
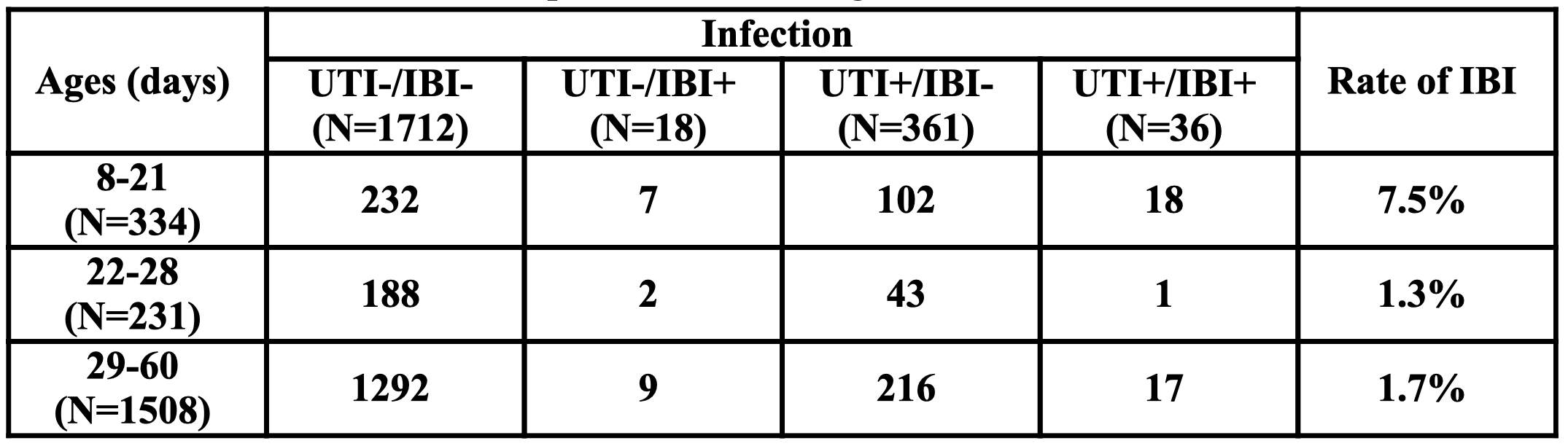 UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); N: Number of patients
UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); N: Number of patients Table 2: Relative Risk of IBI in UTI-positive versus UTI-negative infants by age
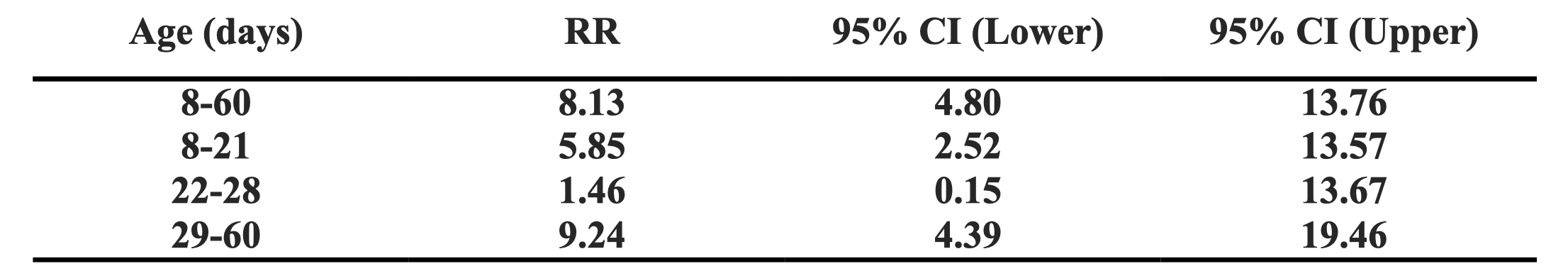 UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); RR: Relative risk; CI: Confidence interval
UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); RR: Relative risk; CI: Confidence interval Table 3: Relative Risk of IBI in UTI-positive infants between age groups
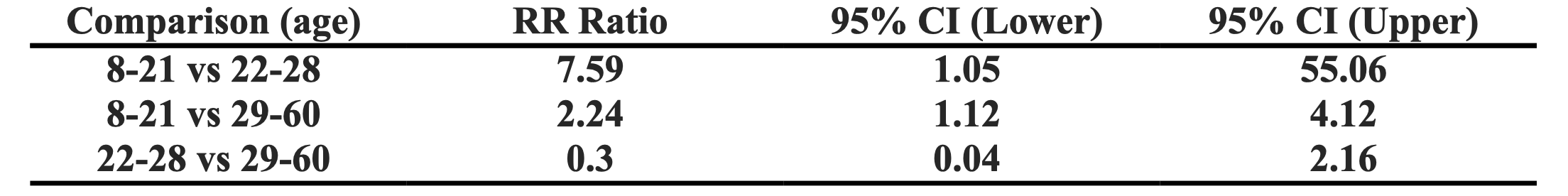 UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); RR: Relative risk; CI: Confidence interval
UTI: Urinary tract infection; IBI: Invasive bacterial infection (bacteremia, meningitis); RR: Relative risk; CI: Confidence interval
