General Pediatrics 2
Session: General Pediatrics 2
719 - Postpartum Depression Screening and Resource Referral in Pediatric Care Settings
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 719.6180
Logan R. McLennan, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Eliana Davis, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Stephanie C. Lux, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Larry Wang, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Krystal Madkins, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Darius Tandon, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States

Logan R. McLennan, Bachelor of Science (he/him/his)
Medical Student
Northwestern University Feinberg School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background: Early identification of postpartum depression (PPD) is essential for the well-being of both mothers and children, as untreated PPD is associated with detrimental effects on a child's cognitive, social, and emotional development. Pediatric care settings can play a vital role in early identification and referral support for PPD given their accessibility and frequent contact with new mothers. Methods to identify and manage PPD in pediatric care clinics vary, however, with some clinics neglecting screening altogether. Understanding existing practices and challenges faced by pediatric care providers can inform the development of guidelines and support systems that ensure mothers receive treatment promptly.
Objective: This scoping review was designed to collate research on screening and referral practices for PPD in pediatric care settings to determine both frequency of and barriers to PPD screening and treatment referral in pediatric settings.
Design/Methods: The search strategy followed the PRSIMA-ScR checklist, and our protocol for study selection was registered prospectively with the Open Science Framework. Abstracts and full texts were assessed by four independent reviewers working in pairs. Disputes were resolved through discussion by all four reviewers.
Studies were included if they focused on screening or referral methods for PPD in mothers with infants under one year accessing care in pediatric outpatient or NICU settings. Only original work published in English was included.
Results: 45 full text articles were identified that met our inclusion criteria [Figure 1]. There was no significant variation in reported screening rates among majority Asian, Black, Hispanic, or White clinics, with an average rate of 79.0% (n=14). Of papers that reported barriers to screening, staff familiarity with protocols was the most cited reason for not screening [Figure 2]. Quality improvement (QI) strategies to support PPD screening and referral were included in 18 studies, and the most popular strategy was staff training (n=8). In papers that examined QI initiatives and directly recorded data on screening rate improvement, the screening rates significantly increased (n=7, p=0.024) [Figure 3]. Detection of PPD also improved after QI, though not significantly (n=6) [Figure 3].
Conclusion(s): While PPD screening in pediatric settings is widely recognized as beneficial, many inconsistencies still exist in clinical practice. Using QI frameworks to train providers and integrate PPD screenings into the pediatric care workflow may increase PPD screening and referral, benefitting both parents and their children.
Flowchart Representation of Search Strategy
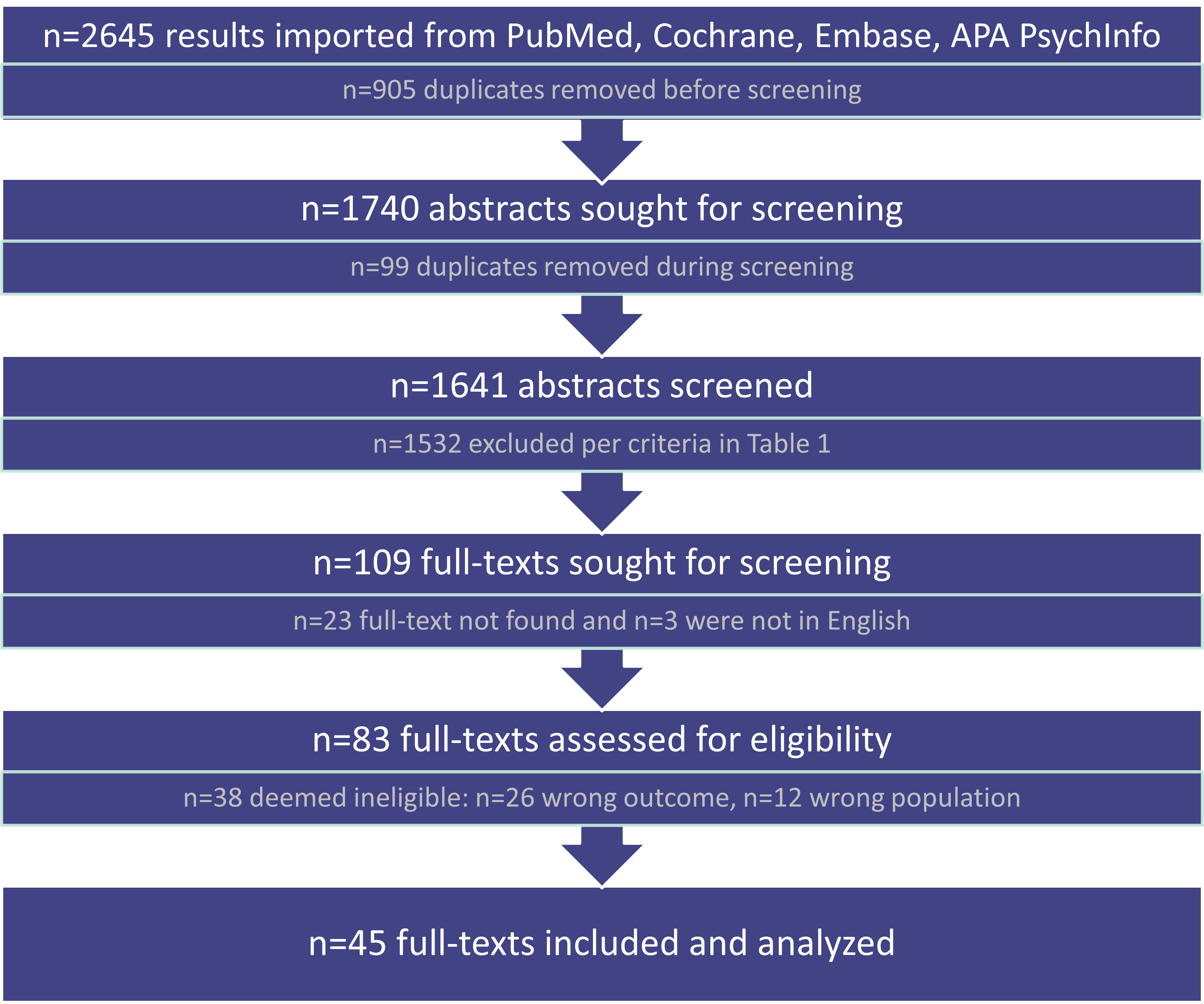 Figure 1: Search strategy used for evaluating texts in the scoping review methodology.
Figure 1: Search strategy used for evaluating texts in the scoping review methodology.Reported Barriers to Screening and Referral
.png) Figure 2: Articles that reported barriers to screening (n=22) and referral (n=9), where the count represents how many articles referenced each individual barrier.
Figure 2: Articles that reported barriers to screening (n=22) and referral (n=9), where the count represents how many articles referenced each individual barrier.Screening Rates and Rates of Depression with Quality Improvement Initiatives
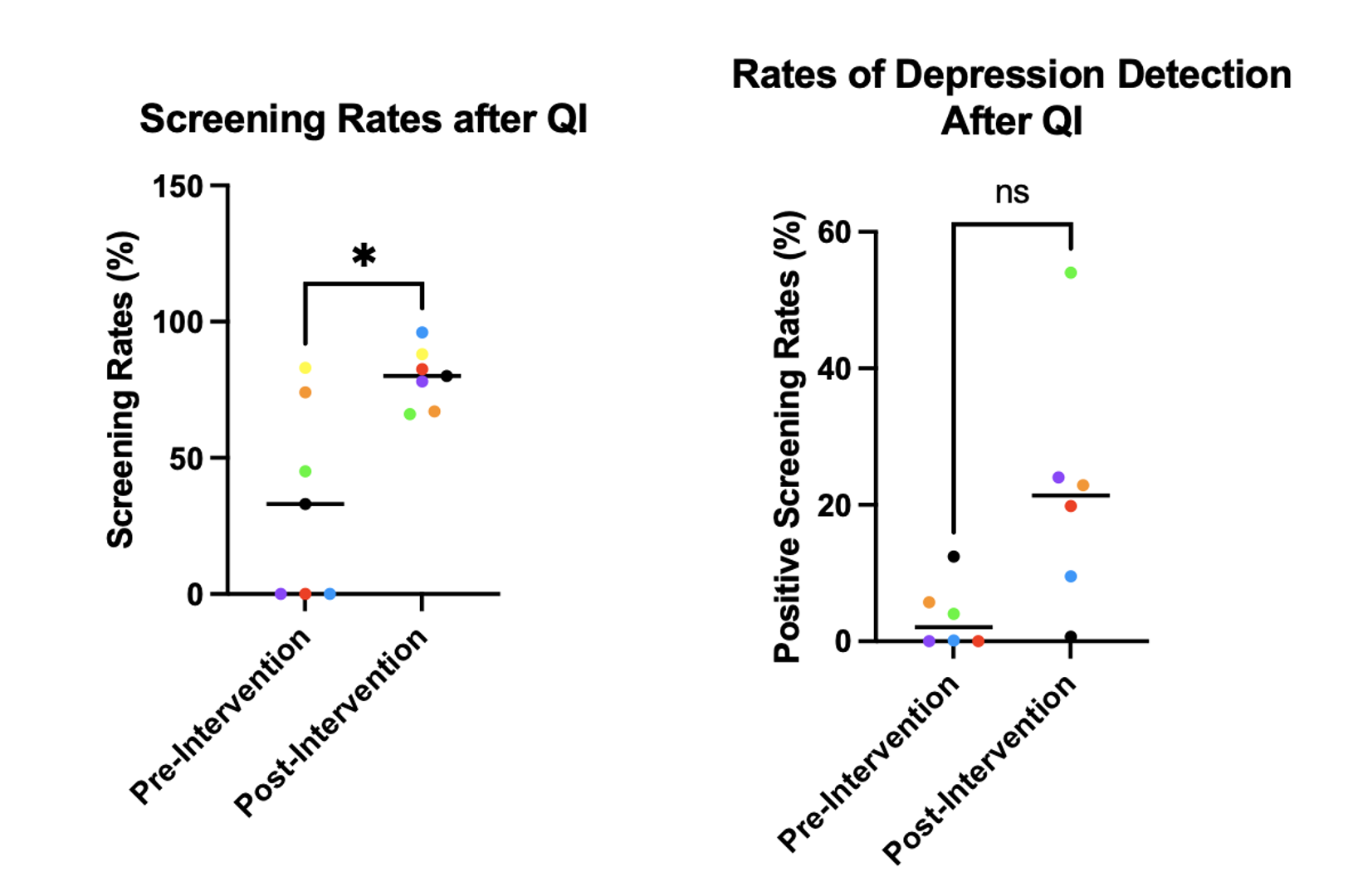 Figure 3: PPD screening rates (n=7) and rates of positive screens (n=6) before and after implementation of QI interventions for providers. QI interventions were individual to each study and not standardized. Each study is represented by a single color and * indicates p < 0.05.
Figure 3: PPD screening rates (n=7) and rates of positive screens (n=6) before and after implementation of QI interventions for providers. QI interventions were individual to each study and not standardized. Each study is represented by a single color and * indicates p < 0.05.

