Neonatal Quality Improvement 2
Session: Neonatal Quality Improvement 2
078 - Reducing Uninformative Respiratory Cultures in the Neonatal/Infant Intensive Care Unit
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 78.6452
Lakshmi Srinivasan, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Danielle Cestare, Children's Hospital of Philadelphia, Ewing, NJ, United States; Alexandra K. Medoro, Perelman School of Medicine at the University of Pennsylvania, Pennsylvania, PA, United States; Jessica L. Rice, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Kathleen Chiotos, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Kathryn Maschhoff, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Daniel Malleske, Perelman School of Medicine, University of Pennsylvania, Rydal, PA, United States; Scott A. Lorch, The Children's Hospital of Philadelphia, Philadelphia, PA, United States; Erik A. Jensen, Lucile Packard Children's Hospital Stanford, San Francisco, CA, United States; Nicolas Bamat, Childrens Hospital of Philadelphia, Swarthmore, PA, United States; Michael A. Padula, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Rachel Lista, Childrens Hospital of Philadelphia, Rutledgw, PA, United States; Bolu Oluwalade, Childrens Hospital of Philadelphia, Philaldelphia, PA, United States; Kenneth P. Smith, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Melissa Duran, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Francis W. Simmons, The Children's hospital of Philadelphia, Cherry HIll, NJ, United States; Iyalla E. Peterside, University of Pennsylvania, Cherry Hill, NJ, United States; Kelle J. Matthews, CHOP, Huntingdon Valley, PA, United States; Kathleen Gibbs, University of Pennsylvania/Children's Hospital of Philadelphia, Philadelphia, PA, United States
- LS
Lakshmi Srinivasan, MBBS MSTR (she/her/hers)
Assistant Professor
The Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Respiratory cultures are utilized to evaluate for ventilator-associated infections in the neonatal/infant intensive care unit (NI/ICU). However, bacterial colonization of endotracheal/tracheostomy tubes often results in a positive respiratory culture, which may be misinterpreted as evidence of bacterial infection and antibiotics prescribed inappropriately.
Objective: Our aim was to decrease rate of respiratory cultures per 100 ventilator days in the NI/ICU by 50% regardless of race, ethnicity, or language by September 2024.
Design/Methods: N/IICU patients with an endotracheal/tracheostomy tube that had a bacterial respiratory culture ordered were included in our project scope. We targeted decreasing the collection of respiratory cultures that likely would not impact patient management/clinical care such as those collected for patients who did not have signs or symptoms of a respiratory infection. PDSA cycles included an education campaign, creation of a guideline flowchart (Figure 1), and initiating revisions to our existing sepsis huddle note (Figure 2).
Our outcome measure is the rate of respiratory cultures per 100 ventilator days. Process measures included percentage of respiratory cultures collected as part of a sepsis evaluation, and percentage of respiratory cultures collected that were associated with a sepsis huddle note stating “change in respiratory status” as a symptom. Balancing measures included the rate of bronchoalveolar lavage (BAL) and rate of viral respiratory panel (RRP) per 100 ventilator days.
Results: The project began in November 2023. Baseline data from August 2022 to October 2023 showed our mean rate of respiratory cultures collected per 100 patient days was 2.02. We observed special cause variation in our data, with a centerline shift to 0.98 respiratory cultures per 100 ventilator days, a 51% decrease (Figure 3).
We did not observe a change in our process measure data, nor a change in rate of BALs per 100 ventilator days. We did observe a downward trend in RRPs per 100 ventilator days from December 2023 to May 2024, likely due to seasonal trends. There were no differences in the outcome measure when stratified by race/ethnicity.
Conclusion(s): We decreased the rate of respiratory cultures obtained in our NICU, reducing waste. Providing clinical guidance and building assessments into existing workflows contributed to our improvement. Future efforts include implementing a strategic sustain plan to hardcode change ideas into our system, utilizing EHR-based strategies such as modifications to NICU sepsis huddle 'smart text' and sepsis order sets
Figure 1: Guideline flowchart for NICU respiratory cultures
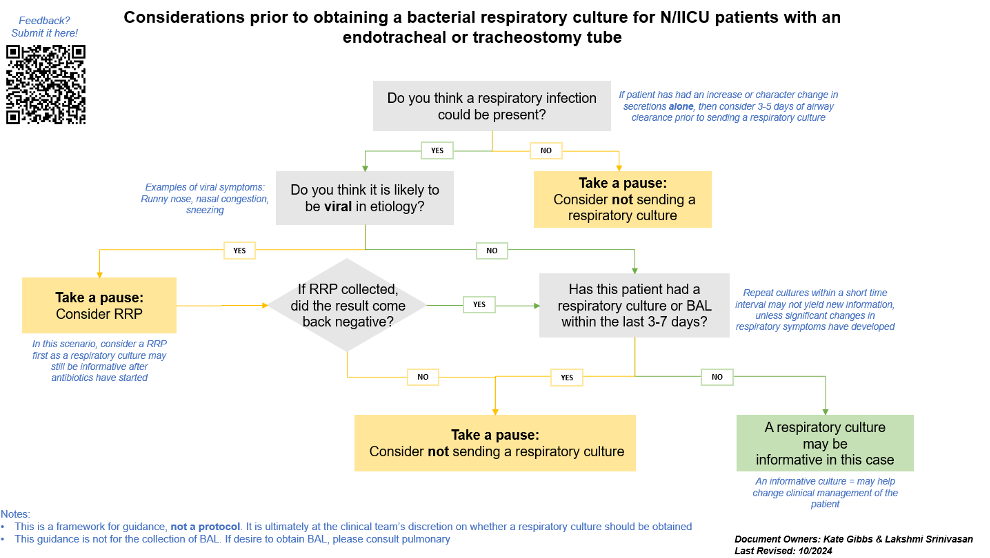
Figure 2: Modifications to 'smart text' in NICU sepsis huddle note
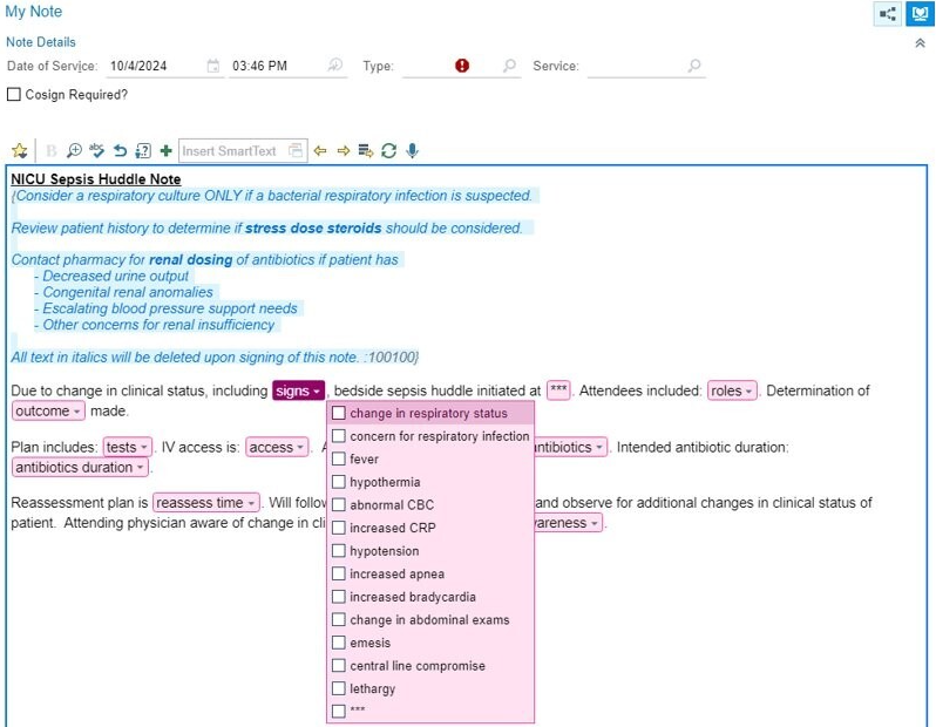
Figure 3: U chart of rate of respiratory cultures per 100 ventilator days
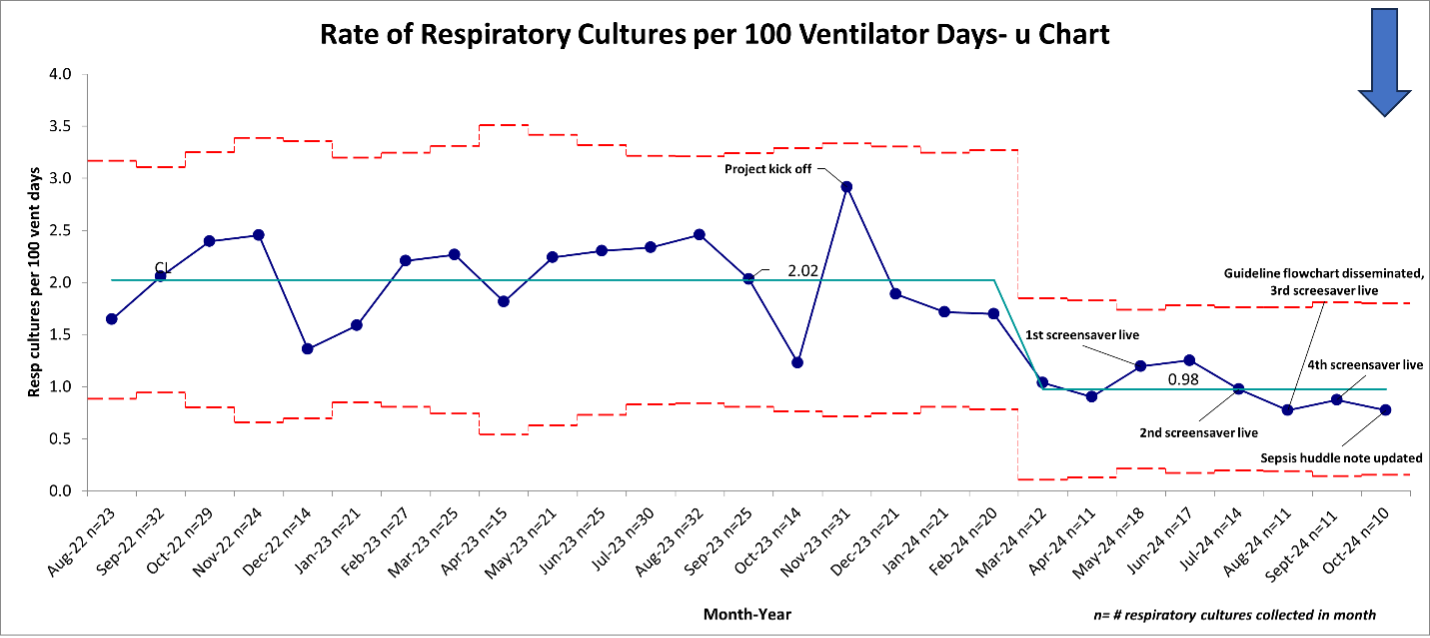 Centerline shift determined to start in March 2024, based on meeting special cause rules and QI team hypothesis about interventions contributing to shift.
Centerline shift determined to start in March 2024, based on meeting special cause rules and QI team hypothesis about interventions contributing to shift.

