General Pediatrics 1
Session: General Pediatrics 1
703 - Trends in Pediatric Providers’ Delivery of Mental and Development Healthcare
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 703.6682
Matthew Mester, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Washington, DC, United States; Elizabeth J. Hisle-Gorman, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Apryl Susi, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Jeanie Kim, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Jeffrey L. Goodie, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States
- EH
Elizabeth Hisle-Gorman, MSW, PhD (she/her/hers)
Associate Professor
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Bethesda, Maryland, United States
Presenting Author(s)
Background: Mental and developmental healthcare provider shortages are impacting care access around the country, and can be especially impactful for those who live in geographically isolated areas.
Objective: We sought to understand trends in pediatrician provision of mental and developmental healthcare throughout the United States annually.
Design/Methods: This cross sectional study used the Military Health System Data Repository to explore the percentage of visits pediatricians are providing mental and developmental healthcare. Care was identified using ICD-10 diagnostic codes and classified into mental and developmental care using the Agency for Healthcare Quality and Research Clinical Classification System, with providers identified using Provider Specialty codes. Joinpoint Analysis examined trends in the provision of mental and developmental care as primary or secondary diagnoses for all pediatric providers on and off military bases.
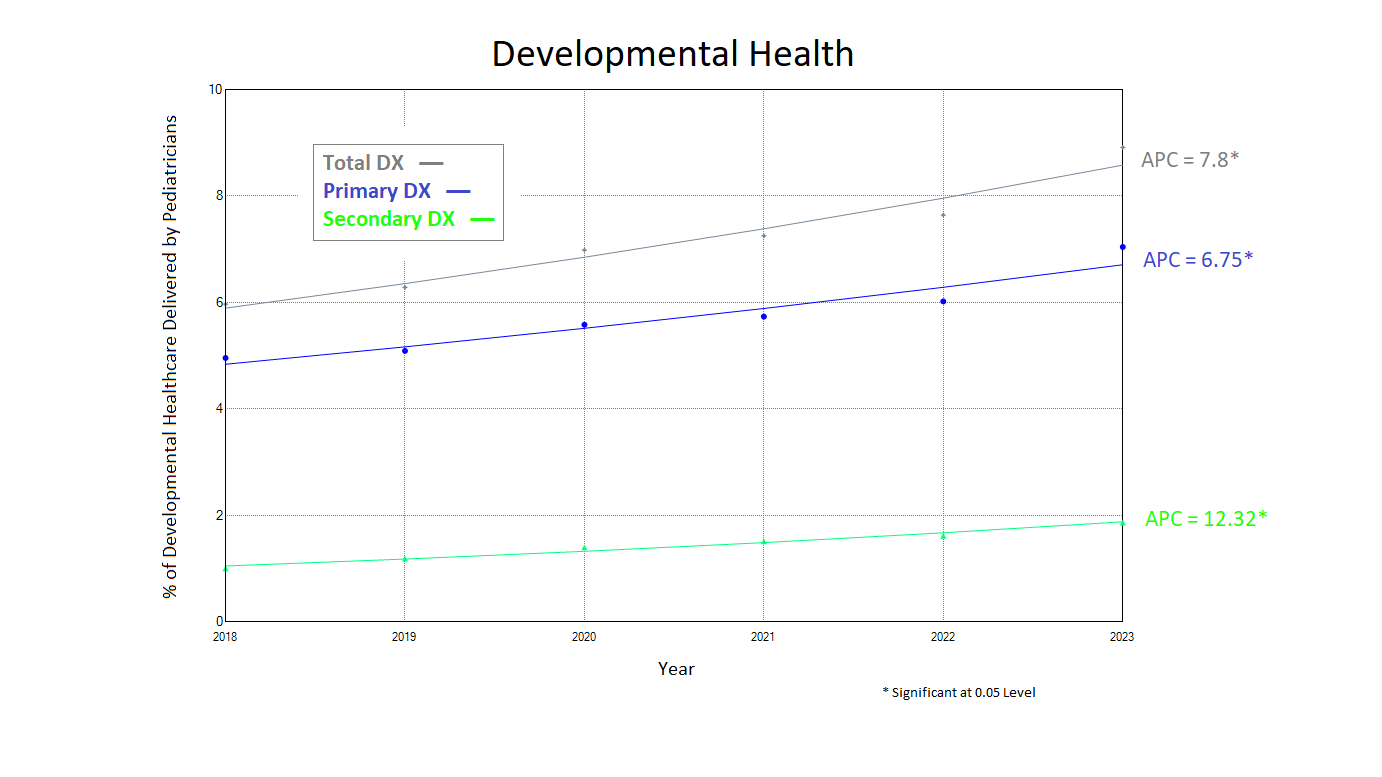
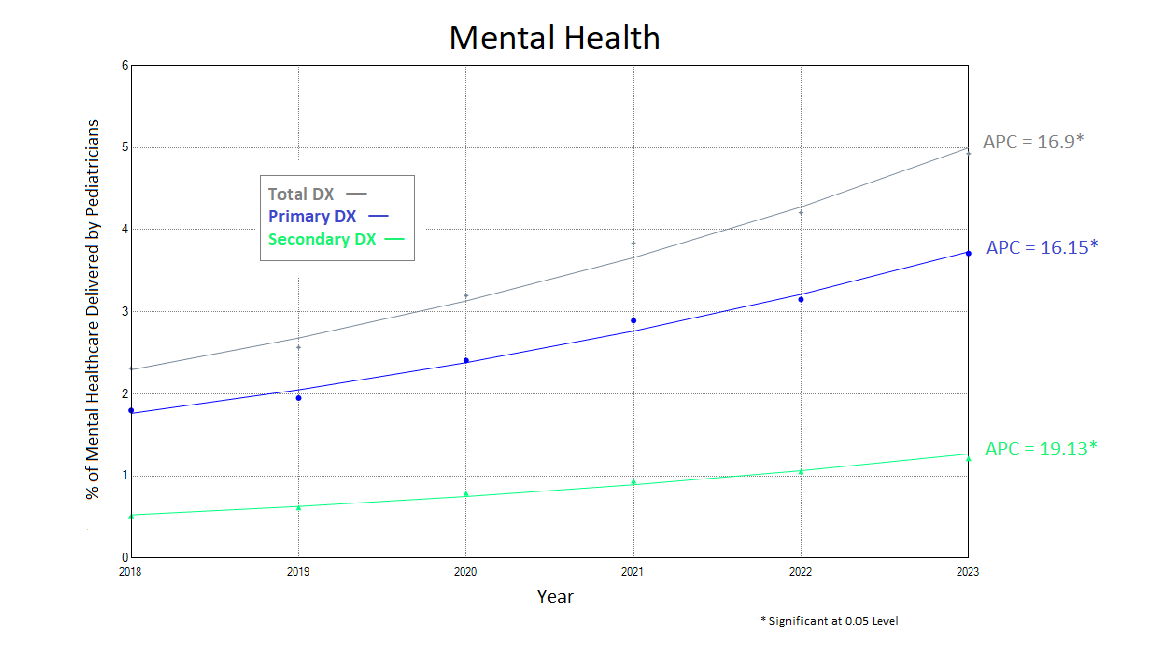
Results: Pediatric providers delivered a median of 8 million outpatient appointments each year from 2018-2022 to children and youth aged 0-25. Over the 6-year course of the study, the percentage of all visits where pediatric providers addressed a mental health diagnosis rose from 2.3 to 4.9% of all visits, a significant annual percent change (APC) of 16.9%. Care increased for visits with a primary diagnosis for mental health (APC=16.2%), and a secondary diagnosis for mental health (APC=19.1%). Care also increased at military treatment facilities (APC=24.3%), and civilian care facilities (11.75%), with a non-significant difference (p=0.07) between the two increased care rates. Developmental care also increased significantly from 6.0 to 8.9% of visits at an annual percent change of 7.8%, and increased for both primary (APC= 6.8%) and secondary diagnoses (APC= 12.3%). Care increased significantly more (p=0.04) at military treatment facilities (APC=11.5%) than civilian providers (APC=5.5%).
Conclusion(s): Pediatricians are spending an increasing proportion of their time providing mental and developmental healthcare to children. Increases are occurring as primary and secondary diagnoses, but with larger increases in secondary diagnoses. Mental health and developmental care provided at military treatment facilities is also increasing more rapidly, suggesting an increased burden on primary care providers at more remote locations. Results suggest the need for additional residency and continuing education training is needed in these disciples.
Overall Comparison of Mental and Developmental Health Trends
.png)
Diagnosis of Mental Health Conditions by Pediatricians Over Time
Diagnosis of Developmental Conditions by Pediatricians Over Time