Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
064 - Transforming NICU Care: A Quality Improvement Initiative to Promote Early Skin-to-Skin Contact
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 64.6651
Emma Prichard, Brooke Army Medical Center, San Antonio, TX, United States; Katrina Savioli, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, San Antonio, TX, United States; Dakota Tomasini, Brooke Army Medical Center, San Antonio, TX, United States
- EP
Emma Prichard, DO (she/her/hers)
Neonatal-Perinatal Fellow
Brooke Army Medical Center
San Antonio, Texas, United States
Presenting Author(s)
Background: Immediate skin to skin care (STSC) for low-birth-weight infants has been associated with a multitude of benefits including a significant improvement in mortality.1 As such, the World Health Organization strongly recommends initiating STSC or kangaroo mother care for preterm or low-birth weight infants as soon as possible after birth.2 Despite this, STSC is often delayed for hours to days after admission to the neonatal intensive care unit (NICU).
Local Problem: Only 40% of infants admitted to our level III NICU received STSC within 12 hours of life.
Objective: Increase the percentage of infants (gestational age >29wks and birth weight >1000g) receiving STSC within 12 hours of life from 40% to 70% in our level III NICU within six months.
Design/Methods: Baseline data was obtained via chart review. A multidisciplinary team of trainee and attending physicians, nurses and leadership was formed to represent key stakeholders in our 20-bed, level III NICU. The primary outcome measure was time from birth to first STSC as recorded in the medical record. Several primary drivers were identified: nursing comfort/confidence, clear guidelines, provider involvement, parental comfort. A multi-faceted intervention over time including parental, provider and nursing education, standardized unit protocol, and bedside visual cues, was developed and implemented. Subsequent plan-do-study-act (PDSA) cycles involved adding key champions, regular staff updates and nursing shout-outs. Descriptive statistics and run charts were used to evaluate and improve the intervention. Balancing measures were adverse events including hypothermia, line mispositioning, accidental extubation or significant desaturation events.
Results: Seventy-two eligible infants were admitted to the NICU during the intervention period. Within six months and through 5 PDSA cycles, the overall percentage of infants receiving STSC by 12 hours of life increased from 40% to 73%. The proportion of infants without any documented STSC decreased from 33% to 8%. The median time to STSC decreased from 15(7.8-24.3) hours to 6.5(3.7-13.7). Corresponding run charts are seen in figures 1 and 2. No adverse events were reported.
Conclusion(s): A multidisciplinary, tiered intervention strategy greatly reduced the time to STSC in our NICU, meeting our AIM for the initiative. This improvement demonstrates the feasibility and effectiveness of a comprehensive approach to promoting early STSC in a complex NICU setting.
FIGURE 1
.png) Run chart depicting the change in percent of infants reaching STSC within 12 hours of life (blue) and number of infants without any skin to skin documented (orange) over time. A) PDSA1 - Educational materials given to nursing and NICU providers B) PDSA 2 - Intervention bundle and new protocol implemented 1JAN C) PDSA3 - Charge nurse champions D) PDSA 4 - Monthly email updates E) PDSA 5 - Nurse shout outs implemented.
Run chart depicting the change in percent of infants reaching STSC within 12 hours of life (blue) and number of infants without any skin to skin documented (orange) over time. A) PDSA1 - Educational materials given to nursing and NICU providers B) PDSA 2 - Intervention bundle and new protocol implemented 1JAN C) PDSA3 - Charge nurse champions D) PDSA 4 - Monthly email updates E) PDSA 5 - Nurse shout outs implemented.FIGURE 2
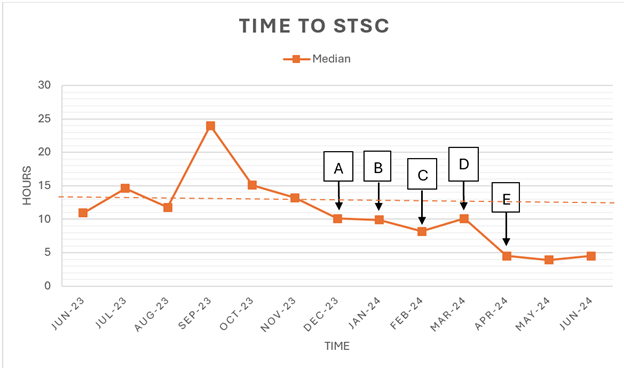 Run chart depicting the change in median time to STSC over time. A-E described in Figure 1.
Run chart depicting the change in median time to STSC over time. A-E described in Figure 1.

