Critical Care 1
Session: Critical Care 1
107 - A Standardized High Frequency Percussive Ventilation (HFPV) Management Pathway and Education Intervention for Neonatal and Pediatric Critical Care Interfacility Transport: A Feasibility Study.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 107.3759
Lindsey L. Scheller, University of California, San Francisco, School of Nursing, los altos, CA, United States; Mandeep Chadha, UCSF Benioff Children's Hospital Oakland, Oakland, CA, United States; Charles Hood, UCSF Benioff Childrens Hospitals, San Francisco, CA, United States; Thomas Hoffmann, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Peter Oishi, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Sandra Staveski, UCSF Benioff Children's Hospital San Francisco, Oakland, CA, United States

Lindsey L. Scheller, PhD(c), BSN, RN (she/her/hers)
Doctoral Candidate
University of California, San Francisco, School of Nursing
los altos, California, United States
Presenting Author(s)
Background: Children with severe acute respiratory failure may require high-frequency percussive ventilation (HFPV) during interfacility transport to quaternary centers. Yet, HFPV is a high-risk, low-volume intervention for clinicians on critical care transport with limited evidence to guide its use during transit.
Objective: To assess changes in clinician knowledge, confidence, and feasibility of an educational intervention and standardized HFPV management pathway during interfacility transport over a 1-year period to a quaternary pediatric hospital.
Design/Methods: We conducted a 1-year pre-post study involving all transport clinicians guided by the Diffusion of Innovation theory. Outcomes were measured at baseline, immediately post-, 4-months, and 8-months post-intervention. The primary outcome was intervention feasibility, with secondary outcomes of confidence and knowledge scores. Feasibility and confidence were measured as a 5-point Likert scale and knowledge was scored out of 5 points. The intervention included 4 educational modules, simulations, and a HFPV management pathway. Multivariable linear mixed models with a non-parametric bootstrap were used to evaluate feasibility, confidence, and knowledge scores over time, adjusting for confounders including gender, position, and years of transport experience.
Results: Of 60 participants, most were female (68%) and worked as physicians (45%) or registered nurses (20%, Table 1). Average baseline scores showed neutral perceptions of feasibility (3.6), confidence (3.1), and knowledge (2.6/5), with increases across all measures post-intervention (Table 2). Multivariable analyses revealed a half point Likert scale increase for feasibility and confidence post-intervention, indicating higher agreement in feasibility and clinician confidence. Compared to the pre-intervention period, feasibility scores increased by 0.57 points (95% CI=0.38-0.79) immediately post-intervention and 0.40 points (95% CI=0.18-0.65) at 4-months. Confidence scores increased by 0.68 points (95% CI=0.48-1.08) immediately post-intervention and by 0.39 points (95% CI=0.10-0.69) at 4-months. Knowledge scores improved significantly post-intervention, increasing by 0.67 points (95% CI=0.33-1.03). No outcome had significant change at 8-months.
Conclusion(s): The HFPV pathway and educational intervention improved clinicians' perceptions of feasibility, confidence, and overall knowledge. These findings highlight the value of structured education in complex care and suggest that periodic reinforcement may be necessary to sustain these gains over time.
Table 1. Clinician Demographics (N=60)
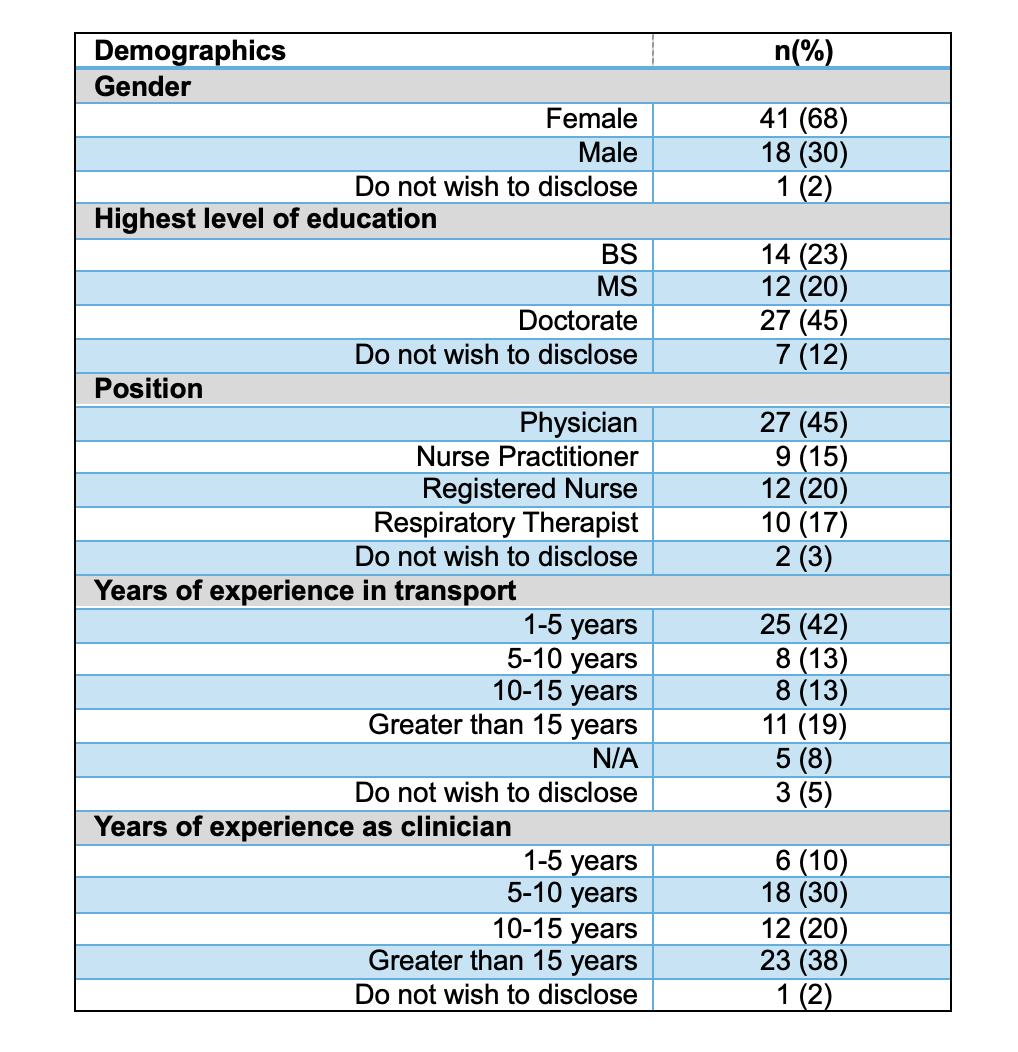
Table 2. Average Feasibility, Knowledge, and Confidence Scores at Baseline and Post-Intervention Time Points
.png)

