Global Neonatal & Children's Health 2
Session: Global Neonatal & Children's Health 2
748 - Severe infection among young infants in Dhaka, Bangladesh: effect of case definition on incidence estimates
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 748.6566
Alastair Fung, The Hospital for Sick Children, Toronto, ON, Canada; Cole Heasley, The Hospital for Sick Children, Toronto, ON, Canada; Lisa G.. Pell, The Hospital for Sick Children, Toronto, ON, Canada; Diego G. Bassani, The Hospital for Sick Children, Toronto, ON, Canada; Prakesh S. Shah, Mount Sinai Hospital, Toronto, ON, Canada; Shaun Morris, Hospital for Sick Children and University of Toronto, Toronto, ON, Canada; Davidson H. Hamer, Boston University School of Public Health, Cambridge, MA, United States; Mohammad Shahidul Islam, Child Health Research Foundation, Dhaka, Dhaka, Bangladesh; Mohammad Abdullah Mahmud, Shield Pharmaceuticals Corp. USA, New York, NY, United States; Eleanor Pullenayegum, The Hospital for Sick Children, Toronto, ON, Canada; Samir K. Saha, Child Health Research Foundation, Dhaka, Dhaka, Bangladesh; Rashidul Haque, icddr,b, Dhaka, Dhaka, Bangladesh; Md Iqbal Hossain, icddr,b, Dhaka, Dhaka, Bangladesh; Chun-Yuan Chen, The Hospital for Sick Children, Toronto, ON, Canada; Abby Emdin, University of Toronto, Toronto, ON, Canada; Karen M. O'Callaghan, King's College London, London, England, United Kingdom; Miranda G. Loutet, The Hospital for Sick Children, Toronto, ON, Canada; Shamima Sultana, International Centre for Diarrheal Disease Research, Bangladesh, Dhaka, Dhaka, Bangladesh; Masum B. Masum, International Centre for Diarrheal Disease Research, Bangladesh, Dhaka, Dhaka, Bangladesh; S M Abdul Gaffar, icddr,b, Dhaka, Dhaka, Bangladesh; Enamul Karim, North South University, Comilla Medical College, Montreal, PQ, Canada; Sharika Sayed, International Centre For Diarrhoeal Disease Research, Bangladesh, Dhaka, Dhaka, Bangladesh; Sultana Yeasmin, icddr,b, Dhaka, Dhaka, Bangladesh; Md Mahbubul Hoque, Bangladesh Shishu Hospita & Institute, Dhaka, Dhaka, Bangladesh; Shafiqul Alam. Sarker, icddr,b, Dhaka, Dhaka, Bangladesh; Daniel Roth, The Hospital for Sick Children, Toronto, ON, Canada

Alastair Fung, MD, MPH (he/him/his)
Clinical Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Severe infections, including sepsis, contribute to a large burden of disease early in life and result in significant morbidity and mortality in young infants ( < 2 months). The burden of sepsis in young infants is particularly high in low- and middle-income countries. Heterogeneity in definitions of severe infection, sepsis and serious bacterial infection (SBI) in young infants limits the comparability of randomized controlled trials (RCTs) of infection prevention and treatment interventions.
Objective: To inform the design of severe infection prevention RCTs for young infants in low-resource settings, we estimated the incidence of severe infection in an observational cohort of Bangladeshi infants aged 0-60 days and examined the effect of variations in case definitions on incidence estimates.
Design/Methods: In 2020-2022, 1939 infants born generally healthy were enrolled at two public hospitals in Dhaka, Bangladesh. Severe infection cases were identified through up to 12 scheduled community health worker home visits from 0-60 days of age or through caregiver self-referral. The primary severe infection case definition combined physician documentation of standardized clinical signs and/or diagnosis of sepsis/SBI and either a positive blood culture or parenteral antibiotic treatment for at least 5 days. Incidence rates were estimated for the primary severe infection definition, the World Health Organization (WHO) definition of possible SBI, blood culture-confirmed infection, and five alternative severe infection definitions.
Results: Severe infection incidence per 1000 infant-days was 1.2 (95% CI 0.97-1.4) using the primary definition, 0.84 (0.69-1.0) using the WHO definition of possible SBI, and 0.026 (0.0085-0.081) using blood culture-confirmed infection (Table 1). Time from birth to severe infection differed by case definition (Figure 1). One-third of cases met the primary criteria for severe infection through physician diagnosis of sepsis/SBI rather than the standardized clinical signs and 85% were identified following caregiver self-referral despite frequent scheduled study visits (Figure 2).
Conclusion(s): Severe infection incidence in young infants varied considerably by case definition. Using a clinical sign-based severe infection definition may miss a substantial proportion of cases identified by physician diagnosis of sepsis/SBI. In settings where health facilities are accessible, and caregivers seek care for infant illness, frequently scheduled home assessments by study personnel to identify severe infection in infants may not be necessary.
Table 1. Incidence proportions and incidence rates of severe infection and variations in severe infection case definition (N=1939 infants)
.png) a At least one sign of possible serious bacterial infection (poor feeding, convulsions, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), lethargy, or fast breathing (>=60 breaths per minute in infants <7 days old)) documented by a study medical officer and non-study treating physician decision to admit to hospital.
a At least one sign of possible serious bacterial infection (poor feeding, convulsions, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), lethargy, or fast breathing (>=60 breaths per minute in infants <7 days old)) documented by a study medical officer and non-study treating physician decision to admit to hospital.b At least one sign of clinical severe infection (poor feeding, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), or lethargy) documented by a study physician and non-study physician decision to admit to hospital.
c At least one sign of critical illness (poor feeding, convulsions, or lethargy) documented by a study physician and non-study physician decision to admit to hospital.
d Not a cumulative sum of severe infection and deaths because 2 infants had severe infection and then died.
e Estimated as 1 minus the survival probability at day 60.
Figure 1. Kaplan-Meier curves for time to severe infection up to 60 days of age according to various severe infection case definitions
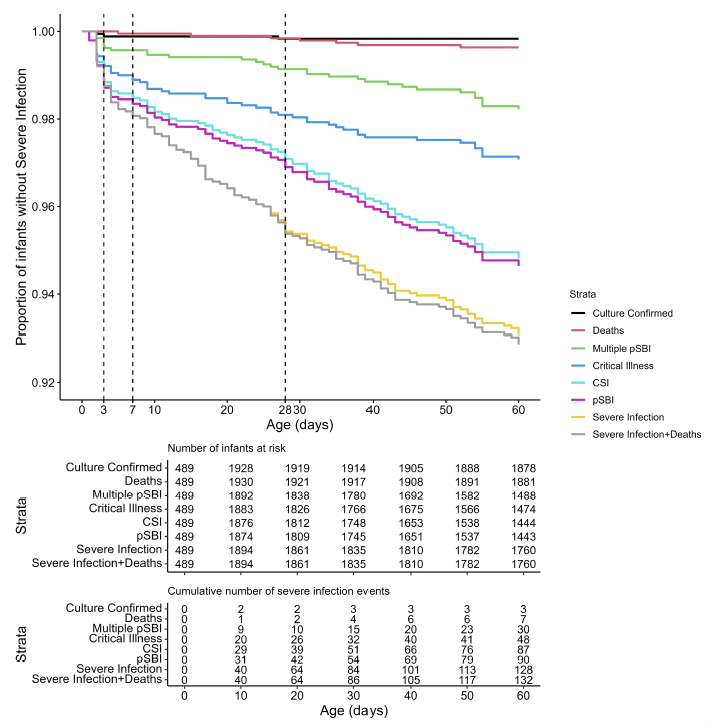 CSI: clinical severe infection; pSBI: possible serious bacterial infection; SI: severe infection.
CSI: clinical severe infection; pSBI: possible serious bacterial infection; SI: severe infection.Note: Number of infants at risk at time 0 (n=489) is lower than at 10 days because infants were enrolled between days 0 to 4 after birth.
Figure 2. Referral pathways by which severe infection episodes were identified within the study
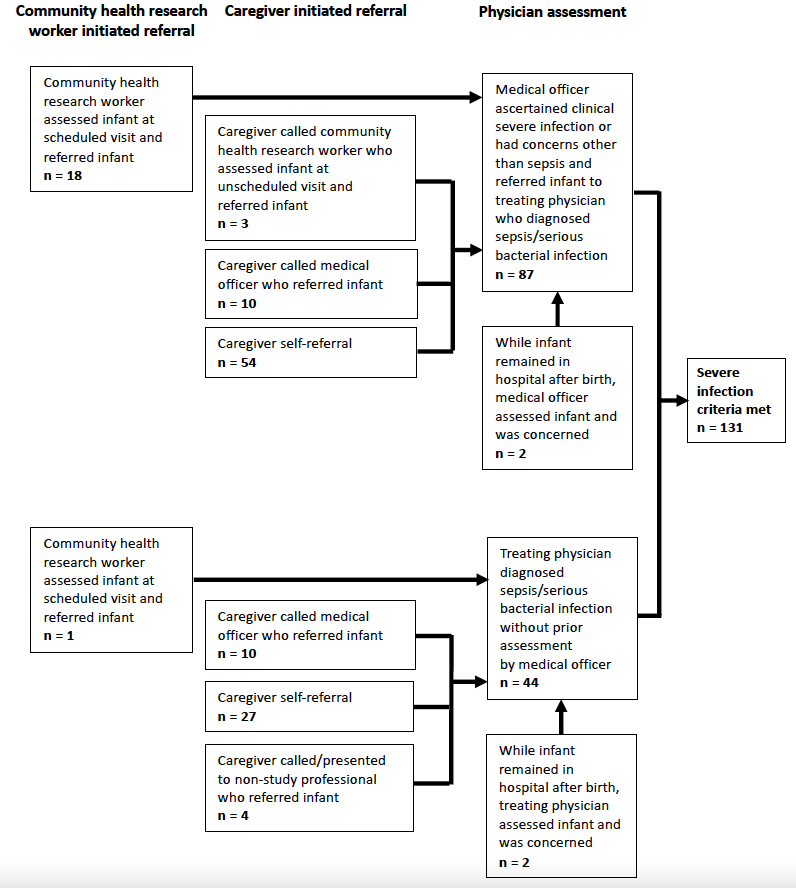 Note: Infants may have had multiple assessments by study and non-study personnel for a severe infection illness episode prior to meeting final severe infection criteria. Frequencies are based on initial presentation and assessment for the severe infection episode.
Note: Infants may have had multiple assessments by study and non-study personnel for a severe infection illness episode prior to meeting final severe infection criteria. Frequencies are based on initial presentation and assessment for the severe infection episode.Table 1. Incidence proportions and incidence rates of severe infection and variations in severe infection case definition (N=1939 infants)
.png) a At least one sign of possible serious bacterial infection (poor feeding, convulsions, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), lethargy, or fast breathing (>=60 breaths per minute in infants <7 days old)) documented by a study medical officer and non-study treating physician decision to admit to hospital.
a At least one sign of possible serious bacterial infection (poor feeding, convulsions, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), lethargy, or fast breathing (>=60 breaths per minute in infants <7 days old)) documented by a study medical officer and non-study treating physician decision to admit to hospital.b At least one sign of clinical severe infection (poor feeding, severe chest indrawing, fever (>=38oC), hypothermia ( <35.5oC), or lethargy) documented by a study physician and non-study physician decision to admit to hospital.
c At least one sign of critical illness (poor feeding, convulsions, or lethargy) documented by a study physician and non-study physician decision to admit to hospital.
d Not a cumulative sum of severe infection and deaths because 2 infants had severe infection and then died.
e Estimated as 1 minus the survival probability at day 60.
Figure 1. Kaplan-Meier curves for time to severe infection up to 60 days of age according to various severe infection case definitions
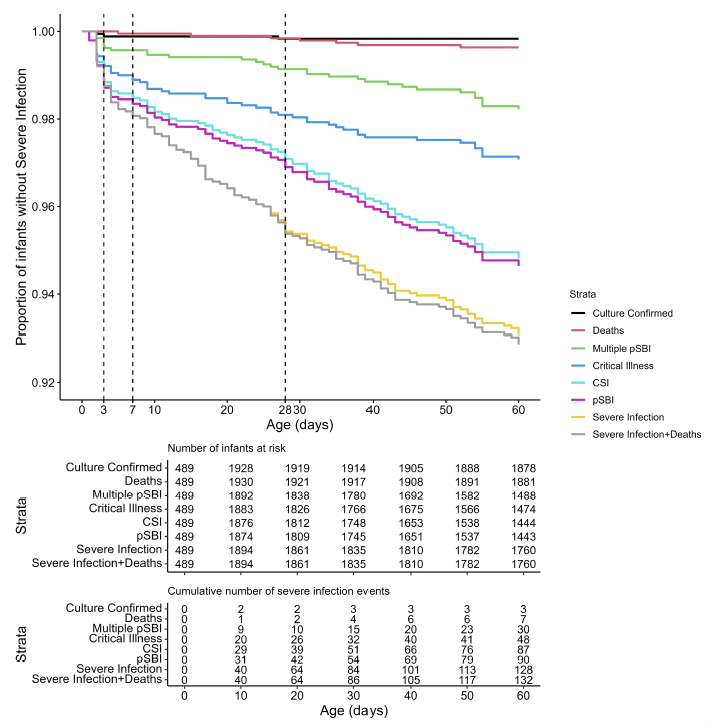 CSI: clinical severe infection; pSBI: possible serious bacterial infection; SI: severe infection.
CSI: clinical severe infection; pSBI: possible serious bacterial infection; SI: severe infection.Note: Number of infants at risk at time 0 (n=489) is lower than at 10 days because infants were enrolled between days 0 to 4 after birth.
Figure 2. Referral pathways by which severe infection episodes were identified within the study
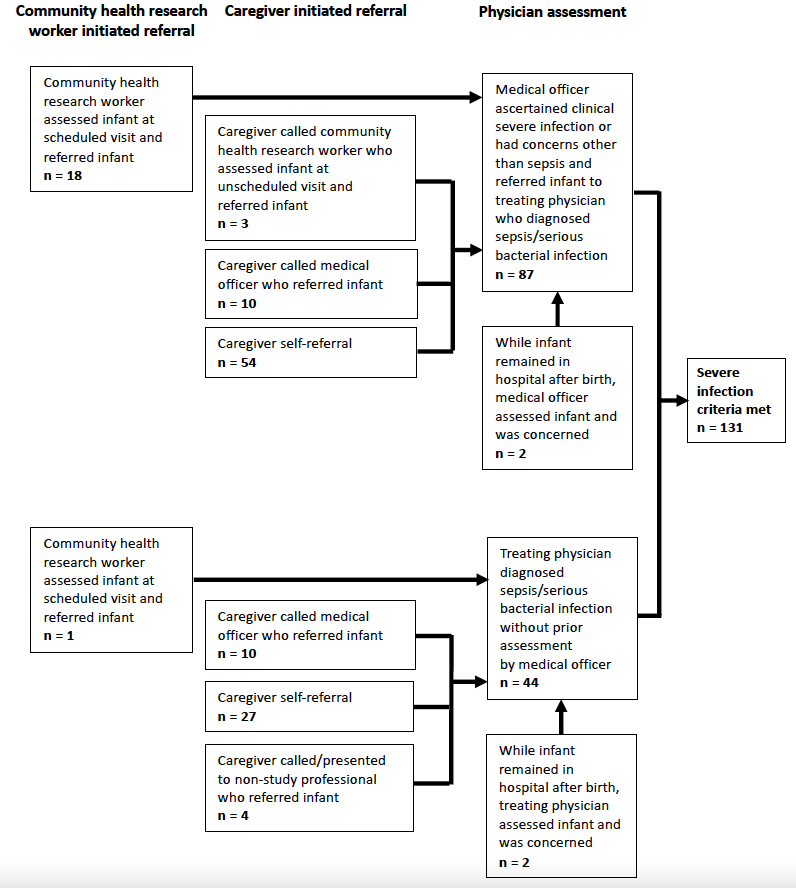 Note: Infants may have had multiple assessments by study and non-study personnel for a severe infection illness episode prior to meeting final severe infection criteria. Frequencies are based on initial presentation and assessment for the severe infection episode.
Note: Infants may have had multiple assessments by study and non-study personnel for a severe infection illness episode prior to meeting final severe infection criteria. Frequencies are based on initial presentation and assessment for the severe infection episode.
