Critical Care 1
Session: Critical Care 1
110 - Assessment of hospital-wide standardized Diabetic ketoacidosis management
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 110.3824
Meghana Kovvuri, Cleveland Clinic Children's, Corpus Christi, TX, United States; Amy Joseph, Cleveland Clinic Children's, Cleveland, OH, United States; Emily Rembetski, Cleveland Clinic Children's, Cleveland Heights, OH, United States; Wei Liu, Cleveland Clinic Foundation - Cleveland, OH, Cleveland, OH, United States; Sumana Narasimhan, Cleveland Clinic Childrens Hospital, Cleveland, OH, United States; Samir Latifi, Cleveland Clinic Children's, Cleveland, OH, United States; Hemant Agarwal, Akron Children's Hospital, Solon, OH, United States

Meghana Kovvuri, MD (she/her/hers)
Pediatric critical care attending
Driscoll Children's Hospital
Corpus Christi, Texas, United States
Presenting Author(s)
Background: ISPAD, NICE and other organizations have issued guidelines for diabetic ketoacidosis (DKA) treatment. Exploration of guidelines in standardized management of hospitalized DKA patients from Emergency department (ED) to discharge is limited.
Objective: To assess role of standardized hospital-wide DKA management in reduction of practice variability in the Emergency Department (ED), Pediatric Intensive Care Unit (PICU) and on the pediatric floor. We also assessed role of standardized management on clinical outcomes and DKA complications.
Design/Methods: A single-center, IRB-approved, retrospective study of DKA patients over 5 years (pre-implementation period: Jan 2016 - Dec 2020; post-implementation period: Jan 2021 - June 2023) was undertaken. Volume of fluid boluses and amount of maintenance intravenous (IV) fluids in ED, early initiation of long-acting insulin, two-bag fluid system and clarity of transition to subcutaneous insulin in PICU, and continuation of IV fluids and mandatory DKA education on pediatric floor were standardized. Demographics, outcomes and complications for the two periods were compared by using Wilcoxon rank sum test for continuous variables and chi-square/Fischer's exact test for categorical variables.
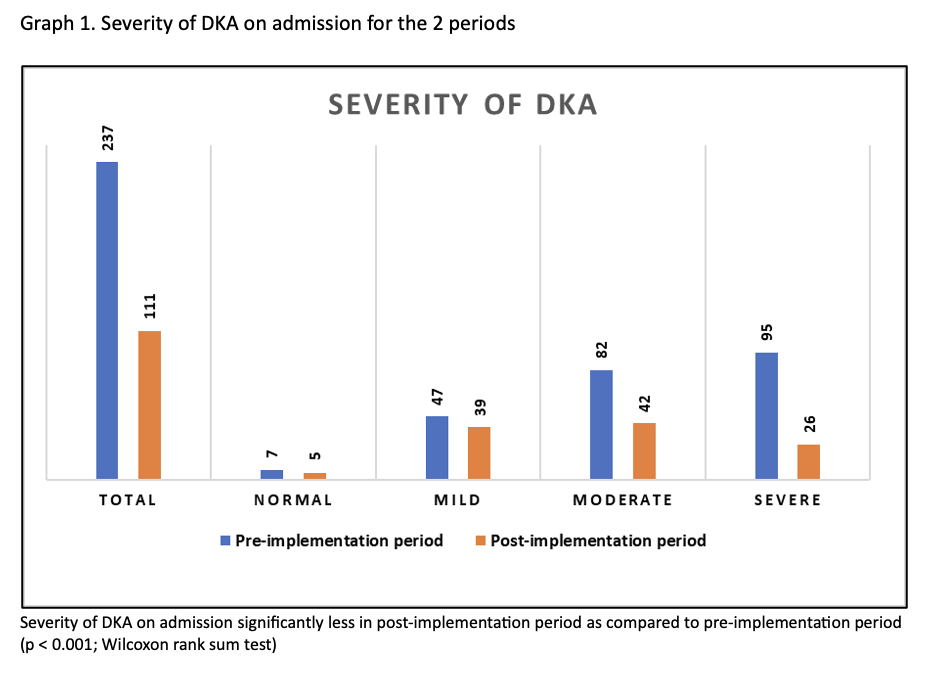
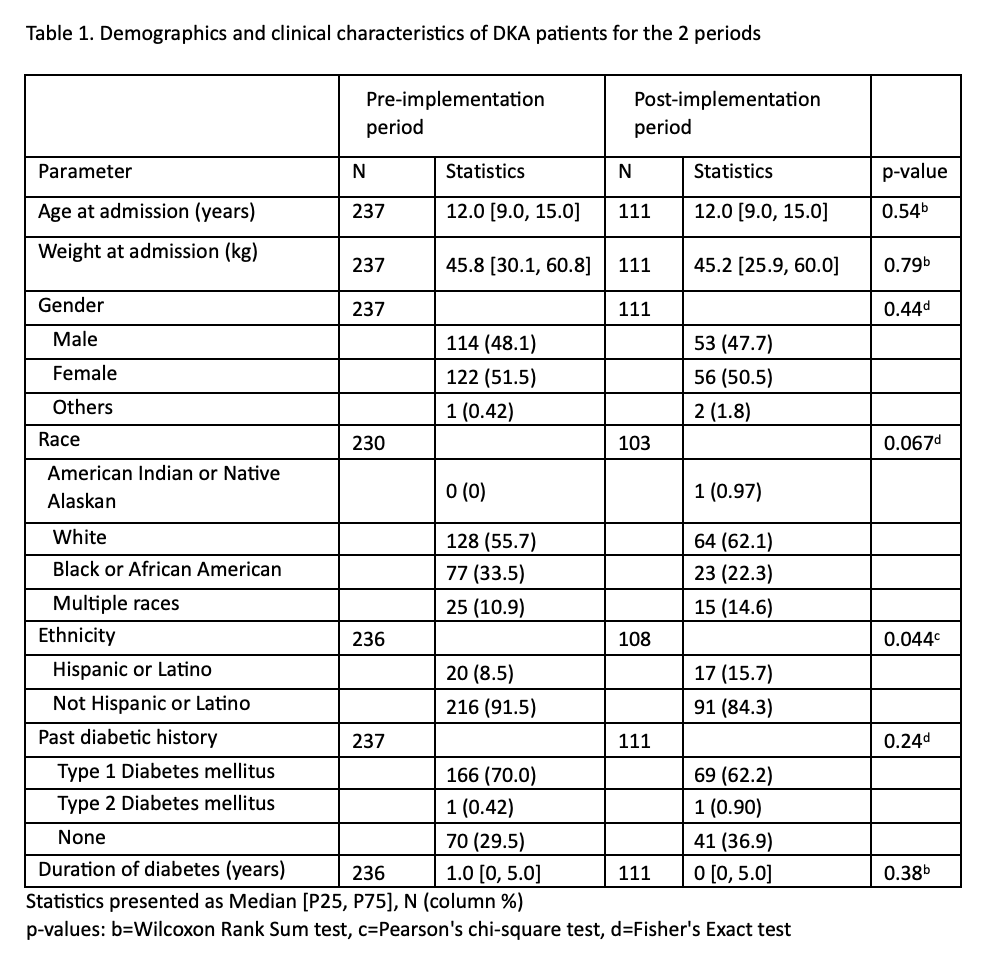
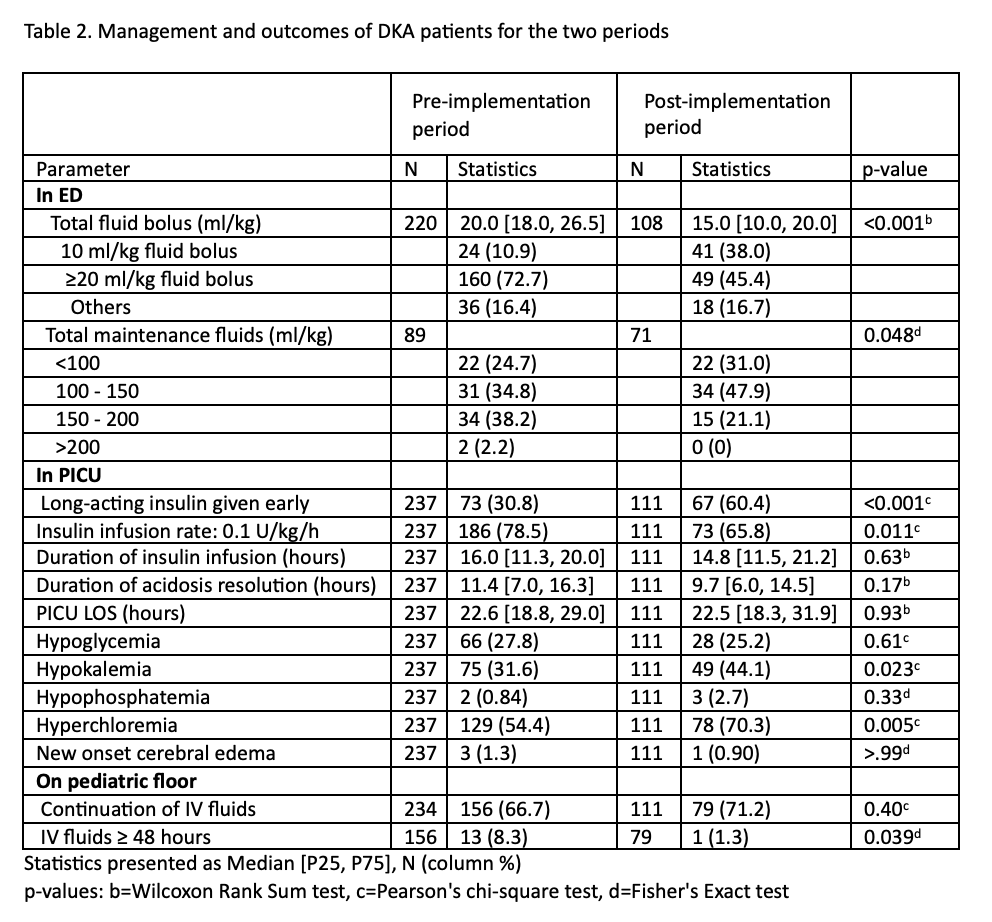
Results: 237 patients in the pre-implementation period were compared to 111 patients in the post-implementation period. Demographics were fairly similar for the two periods (Table 1). In the post-implementation period, patients received lower volume of fluid boluses, and more appropriate initiation of maintenance fluids in ED; more patients received earlier long-acting insulin and less received 0.1 U/kg/h insulin in PICU; and less patients received IV fluids for ≥ 48 hours on pediatric floor (Table 2). Time for acidosis resolution, duration of PICU stay, incidence of hypoglycemia and cerebral edema were similar for the two periods whereas hypokalemia and hyperchloremia were higher in the post-implementation period (Table 2). Generalized linear regression analysis revealed 20% increase in hospital stay in the post-implementation period (mean ratio = 1.2, 95% CI 1.0–1.4, p = 0.019). There was a significant reduction in the DKA severity at presentation in the post-implementation (Graph 1).
Conclusion(s): Standardization of hospital-wide DKA management is associated with reduced practice variability. Early administration of long-acting insulin in DKA management is safe without an increased incidence of hypoglycemia or cerebral edema. Standardized DKA management incorporating diabetes education may play a role in reduction of DKA severity on admission.
Demographics and clinical characteristics of DKA patients for the two periods
Management and outcomes of DKA patients for the two periods
Severity of DKA on admission for the two periods