Allergy, Immunology, and Rheumatology 2
Session: Allergy, Immunology, and Rheumatology 2
648 - Characterization of Myeloid-Derived Suppressor Cells (MDSC) in a Cohort of Healthy Children
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 648.4087
Sara E. Mertz, Nationwide Children's Hospital, Columbus, OH, United States; Dylan J. Brown, Nationwide Children's Hospital, Columbus, OH, United States; Toni Kuhns, Ohio University Heritage College of Osteopathic Medicine, Athens, OH, United States; Michael Tobias, Nationwide Children's Hospital, Dublin, OH, United States; Julie Rice-Weimer, Nationwide Children’s Hospital, Columbus, OH, United States; Lisa M. Steele, Nationwide Children's Hospital, Columbus, OH, United States; Lauren Whang. Donabedian, Nationwide Children's Hospital, Columbus, OH, United States; Julie Breuer, Nationwide Children's Hospital, Columbus, OH, United States; Jill Popelka, Nationwide Children's Hospital, Columbus, OH, United States; Sidhant Kalsotra, Ohio State University College of Medicine, Columbus, OH, United States; Rebecca Glowinski, Nationwide Children's Hospital, Columbus, OH, United States; Katherine Bline, Nationwide Children's Hospital, Bexley, OH, United States

Sara E. Mertz, B.S. (she/her/hers)
Clinical Research Program Coordinator
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Myeloid-derived suppressor cells (MDSC) represent a heterogenous, immunosuppressive cell population that potently suppress T cells and contribute to the compensatory anti-inflammatory response in the host. Prior studies show MDSC can comprise up to 70% of peripheral blood in critically ill children. Healthy adults typically have less than 2% MDSC (or 200 cells/µl) in peripheral blood, however the proportion of MDSC in the peripheral blood mononuclear cell fraction (PBMC) in healthy children is unknown.
Objective: The object of this study was to better understand the MDSC population in healthy children.
Design/Methods: We performed an observational study at Nationwide Children’s Hospital. Subjects were eligible for inclusion if < 18 years without known immune suppression, born > 35 weeks GA, afebrile and at baseline healthy in the 14 days prior to screening. Subjects were recruited in pre-op areas prior to elective, outpatient procedures or through response to an advertisement. PBMC were isolated by ficoll and stained to identify MDSC by flow cytometry. Absolute numbers of MDSC were normalized to the white blood cell count analyzed from the same sample. Nasopharyngeal (NP) viral swabs were for viral PCR testing.
Results: We enrolled 150 children between June 2023- August 2024; 98 (65%) were male, with a median age of 50 [IQR 14,89] months. The median white blood cell count was 7.5 [6.2, 9.7] x103/ µl cells, anesthetic time was 2 [2.0, 3.0] minutes, % MDSC of PBMC was 6.7 [4.4, 11]% and absolute MDSC was 396 [65, 634] cells / µl. No significant difference was observed in the % or absolute number of MDSC according to age (Figure 1A, B), anesthetic time (Figure 2A,B), or by comorbidity (Figure 3A,B). 129 subjects underwent NP swab testing, 29 were positive for one virus, and 10 were positive for more than one virus. The most common detected virus was rhinovirus (n=31). No differences in % or absolute number of MDSC were observed in children with or without a virus (6.3 [4.5, 7.8]% vs 6.8 [4.2, 11]%, p=0.4) and (524 [364, 635] vs 458 [218,717] cells/ µl, p=0.4), respectively.
Conclusion(s): In a cohort of healthy children, the median % and absolute number of MDSC were higher than reported in adults. The % and absolute MDSC were not associated with increasing age, anesthetic time, comorbidity or detected virus. A higher frequency of MDSC in children may play an important role in their immune response to infection. MDSC are a potential therapeutic target and further investigation of the MDSC population is imperative to better understand the maturation of the immune response.
Figure 1. MDSC numbers do not vary by age
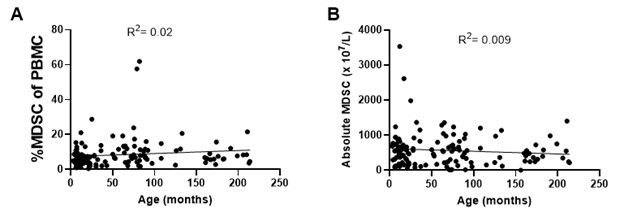 No differences were observed in the (A) percentages of MDSC of peripheral blood mononuclear cells (PBMC) or (B) absolute numbers of MDSC according to age.
No differences were observed in the (A) percentages of MDSC of peripheral blood mononuclear cells (PBMC) or (B) absolute numbers of MDSC according to age.Figure 2. MDSC frequencies do not vary by anesthetic time
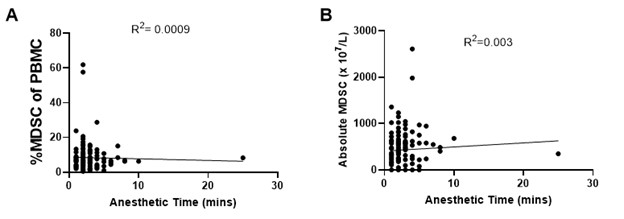 No association was observed in the (A) percentages of MDSC of PBMC or (B) absolute numbers of MDSC with increasing anesthetic time.
No association was observed in the (A) percentages of MDSC of PBMC or (B) absolute numbers of MDSC with increasing anesthetic time. Figure 3. Frequencies of MDSC did not vary by comorbidity
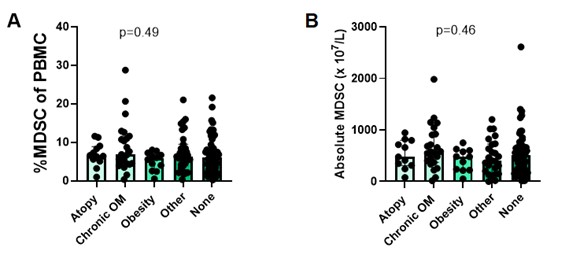 Children with history of atopy (n=12), chronic OM (n=24), obesity (n=10), or other comorbidities (n=28) had similar both (A) percentages MDSC of PBMC and (B) absolute MDSC compared to children without known comorbidities (n=63). OM= otitis media.
Children with history of atopy (n=12), chronic OM (n=24), obesity (n=10), or other comorbidities (n=28) had similar both (A) percentages MDSC of PBMC and (B) absolute MDSC compared to children without known comorbidities (n=63). OM= otitis media. Figure 1. MDSC numbers do not vary by age
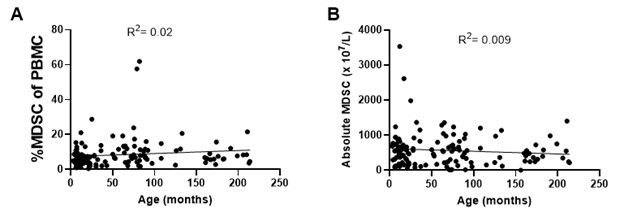 No differences were observed in the (A) percentages of MDSC of peripheral blood mononuclear cells (PBMC) or (B) absolute numbers of MDSC according to age.
No differences were observed in the (A) percentages of MDSC of peripheral blood mononuclear cells (PBMC) or (B) absolute numbers of MDSC according to age.Figure 2. MDSC frequencies do not vary by anesthetic time
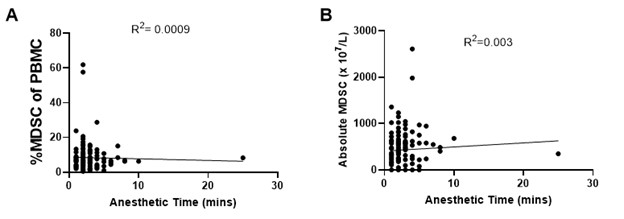 No association was observed in the (A) percentages of MDSC of PBMC or (B) absolute numbers of MDSC with increasing anesthetic time.
No association was observed in the (A) percentages of MDSC of PBMC or (B) absolute numbers of MDSC with increasing anesthetic time. Figure 3. Frequencies of MDSC did not vary by comorbidity
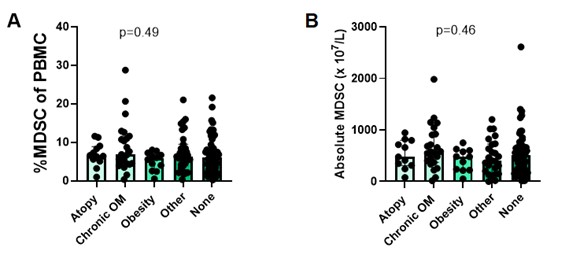 Children with history of atopy (n=12), chronic OM (n=24), obesity (n=10), or other comorbidities (n=28) had similar both (A) percentages MDSC of PBMC and (B) absolute MDSC compared to children without known comorbidities (n=63). OM= otitis media.
Children with history of atopy (n=12), chronic OM (n=24), obesity (n=10), or other comorbidities (n=28) had similar both (A) percentages MDSC of PBMC and (B) absolute MDSC compared to children without known comorbidities (n=63). OM= otitis media. 
