Emergency Medicine 3
Session: Emergency Medicine 3
436 - Contamination Rates of Blood, Urine, and Cerebrospinal Fluid Culture Among Hypothermic Infants Evaluated in the Emergency Department
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 436.4061
Kelly R.. Bergmann, Children’s Minnesota, University of Minnesota Masonic Children’s Hospital, Minneapolis, MN, United States; Amy D. Thompson, Nemours Children's Hospital, Wilmington, DE, United States; Alexandra Geanacopoulos, Boston Children's Hospital, Boston, MA, United States; Nathan Money, University of Utah School of Medicine, Salt Lake City, UT, United States; Stacey L. Ulrich, Rady Children's Hospital San Diego, san diego, CA, United States; Theodore Heyming, CHOC Children's Hospital of Orange County, Orange, CA, United States; Andrea T. Cruz, Baylor College of Medicine, Houston, TX, United States; Paul L. Aronson, Yale School of Medicine, New Haven, CT, United States; Wendi Wendt, Medical College of Wisconsin, Milwaukee, WI, United States; Alexander Rogers, University of Michigan Medical School, Ann Arbor, MI, United States; Leslie Ann. Hueschen, Children's Mercy Hospital/ University of Missouri-Kansas City, Kansas City, MO, United States; Laura F. Sartori, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; Oluwakemi Badaki-Makun, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Naghma S. Khan, Emory University School of Medicine, ATLANTA, GA, United States; Jamie Holland, Medical College of Wisconsin, Milwaukee, WI, United States; Amy Zhou, University of Texas Southwestern Medical School, Dallas, TX, United States; Paria M. Wilson, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sriram Ramgopal, Ann & Robert H. Lurie Children's Hospital of Chicago, Oak Park, IL, United States
- KB
Kelly R. Bergmann, DO, MS (he/him/his)
Pediatric Emergency Physician, Emergency Research Director
Children's Minnesota
Minneapolis, Minnesota, United States
Presenting Author(s)
Background: Infants with hypothermia undergo testing to evaluate for urinary tract infection (UTI) and invasive bacterial infection (IBI), including bacteremia and meningitis. While culture contamination can lead to unnecessary antibiotic exposure and hospitalization, little is known about the frequency of culture contamination in this population.
Objective: We sought to characterize the frequency of urine, blood, and cerebrospinal fluid (CSF) culture contamination among hypothermic infants.
Design/Methods: We conducted a retrospective, cross-sectional cohort study among infants 0-90 days of age with hypothermia (≤36.5°C rectally) presenting to 16 participating Pediatric Emergency Medicine Collaborative Research Committee emergency departments (EDs) between January 1, 2013 to December 31, 2022. Our primary outcome was growth of a contaminant organism on urine, blood or CSF cultures. Culture positivity and contamination were defined according to the established criteria, with expert adjudication for indeterminate cases. We evaluated the most common contaminant organisms from each culture source site, and calculated the false positive rate (FPR) and positive predictive value (PPV) with corresponding 95% confidence intervals (CIs).
Results:
Results: We identified 45,673 eligible encounters among infants with hypothermia [52.9% male, median age 25 days (IQR 6-52)], of which 11,641 (25.5%) had at least one culture obtained. Among infants with cultures obtained, 9,120 (78.3%) had urine, 9,361 (82.0%) had blood, and 4,470 (38.4%) had CSF cultures. Bacterial growth was identified in 744 (8.2%) urine, 397 (4.2%) blood, and 103 (2.3%) CSF cultures. Of cultures with any bacterial growth, 491 (66.0%) urine, 311 (78.3%) blood, and 79 (76.7%) CSF cultures grew contaminant organisms (Figure 1). In contrast, 253 (34.0%) urine, 86 (21.7%) blood, and 24 (23.3%) CSF cultures grew pathogenic organisms. The most common contaminants were polymicrobial species from urine, and coagulase-negative staphylococci from blood and CSF (Table 1). Overall, the FPR was 5.5% (5.4%, 5.6%) for urine, 3.5% (3.4%, 3.6%) for blood, and 1.7% (1.6%, 1.8%) for CSF. The PPV was 34.0% (32.1%, 36.0%) for urine, 21.7% (19.9%, 23.6%) for blood, and 23.3% (19.6%, 27.4%) for CSF.
Conclusion(s): Most culture growth from infants with hypothermia represented false positives. Our findings may inform the interpretation of culture results, particularly when preliminary information is available to treating clinicians, and underscore the need for ongoing efforts to reduce culture contamination.
Table 1. Organisms identified as contaminants by culture type
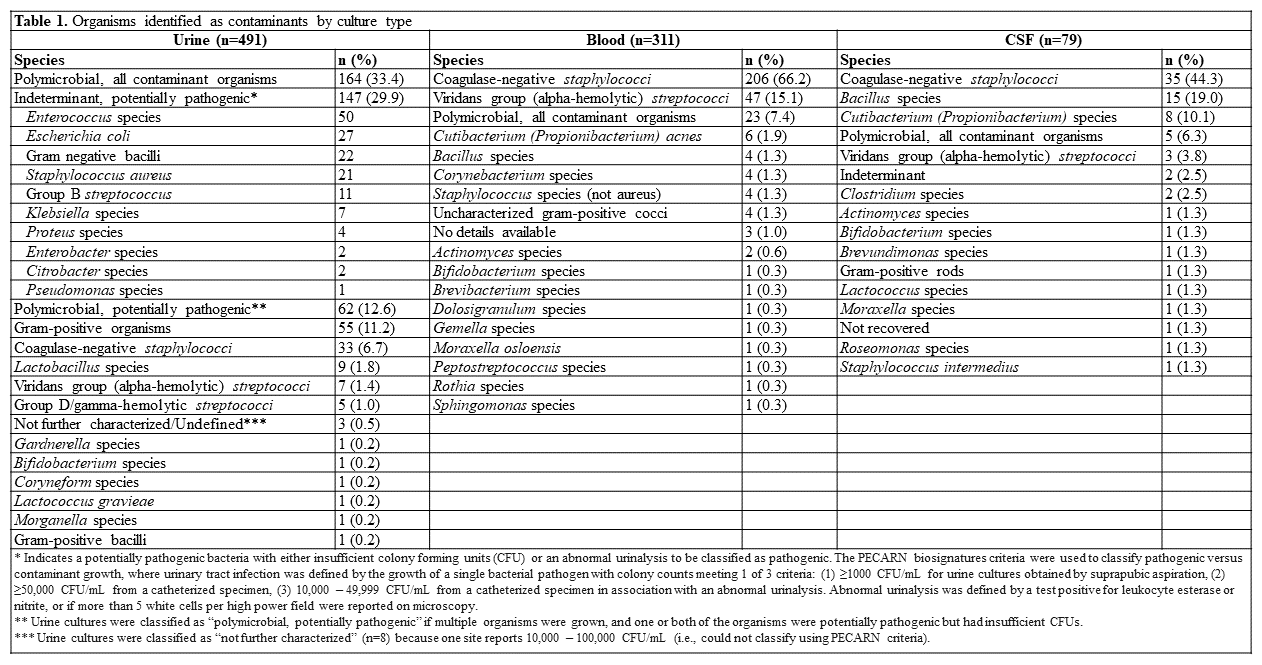
Figure 1. False positive and true negative culture studies by hospital, limited only to cultures with any growth (e.g. contaminant or pathogen)
.png)
Table 1. Organisms identified as contaminants by culture type
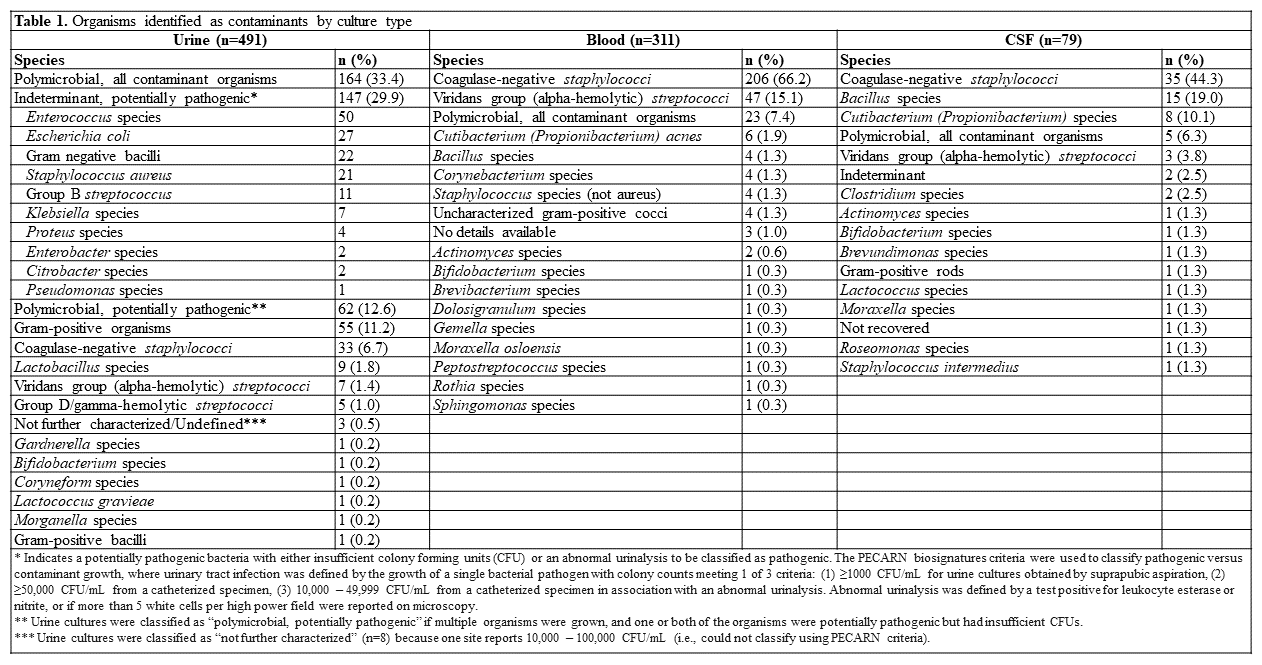
Figure 1. False positive and true negative culture studies by hospital, limited only to cultures with any growth (e.g. contaminant or pathogen)
.png)

