Cardiology 2
Session: Cardiology 2
153 - Evaluating Acute Kidney Injury in Critically Ill Infants After Cardiac Catheterization
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 153.4949
Haleigh N. McBride, Duke University Medical Center, Durham, NC, United States; Sam Littlejohn, Duke University School of Medicine, Durham, NC, United States; Reid Chamberlain, Duke University Hospital, Durham, NC, United States; Gregory A. Fleming, Duke University School of Medicine, Durham, NC, United States

Haleigh N. McBride, DO (she/her/hers)
Resident
Duke University
Durham, North Carolina, United States
Presenting Author(s)
Background: Severe congenital disorders, particularly heart disease (CHD), often require intervention, with 1 in 4 needing catheterization or surgery within their first year. Acute kidney injury (AKI) has been associated with contrast exposure, and raises morbidity and mortality risk in the critically ill pediatric population. Data on post-procedural AKI in infants with CHD undergoing cardiac catheterization is limited.
Objective: This study seeks to describe the incidence of AKI after cardiac catheterization in critically ill infants, identify risk factors for post-procedural AKI, and assess the effect of AKI on post-procedural length of stay (LOS) and in-hospital mortality.
Design/Methods: A retrospective cohort study performed in critically ill infants who underwent cardiac catheterization at a single academic center from 2013-2018. Patients included were < 1 year of age at the time of catheterization and admitted to the ICU post-procedure. Those excluded had insufficient data to diagnose AKI. Using Kidney Disease: Improving Global Outcomes criteria, AKI was defined by change in creatinine within 7 days post-procedure. A multivariate logistic regression model identified patient and procedural risk factors associated with AKI. The relationship between AKI and post-procedural LOS and in-hospital mortality was analyzed by ANOVA and chi-squared test.
Results: Of 313 catheterizations performed in 223 patients, the average age was 95 (±84) days and weight 4.6 (±1.6) kg. The most common diagnosis was cyanotic single ventricle 33.1% (74/223),
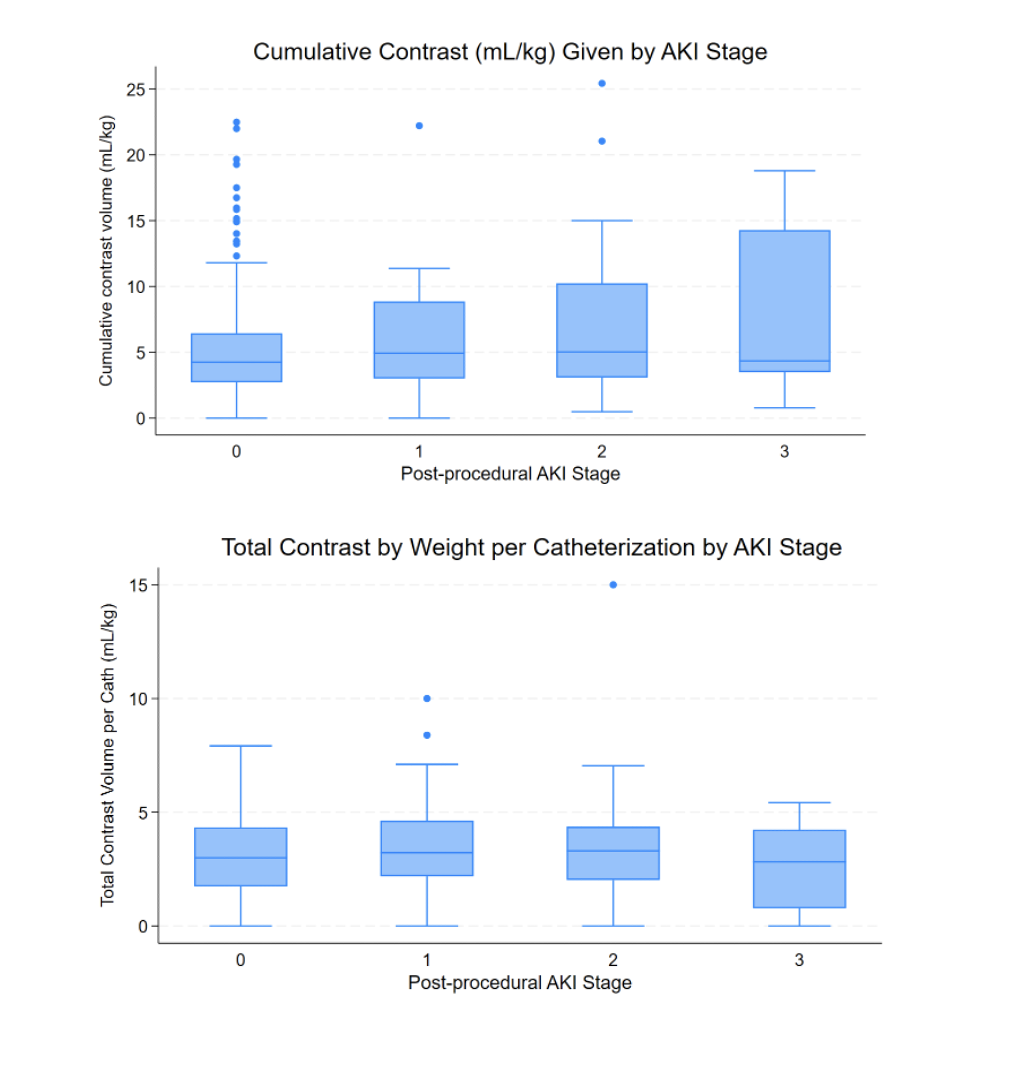
with 57.8% (181/313) exposed to diuretics pre-procedure, 34.2% (107/313) requiring inotropic support, and 41.9% (131/313) undergoing prior cardiac surgery. 31.6% (99/313) of patients developed AKI, with majority stage I (Fig 1). Cumulative contrast exposure, but not per-case exposure was associated with AKI (p=0.022 vs 0.551, Fig 2). Multivariate analysis showed significant associations with increased age (days) at time of catheterization (aOR 1.005; 1.001-1.008, p=0.008) and ECMO exposure (aOR 1.5979; 1.057-2.358, p=0.026), but not contrast exposure. No significant correlation was found between AKI and post-procedural LOS (p=0.2781) or in-hospital mortality (p=0.495).
Conclusion(s): Post-procedural AKI is common after cardiac catheterization in critically ill infants. Factors of intrinsic risk or hemodynamic instability may pose a more significant risk for AKI than contrast exposure. Unlike post-operative AKI, post-procedural AKI does not appear to be associated with increased LOS or mortality.
Fig 1: Proportion of Critically Ill Infants Developing Acute Kidney Injury (AKI) by Stage After Cardiac Catheterization
.png)
Fig 2: The Relationship between Cumulative Contrast Exposure and Per-Case Contrast Exposure with Acute Kidney Injury (AKI) Stage