General Pediatrics 1
Session: General Pediatrics 1
693 - Examining Protocols in Practice: Screening and Response Rates for Postpartum Depression in a Primary Care Setting
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 693.4610
Nicole Heredia, Boston Children's Hospital, Boston, MA, United States; Alexandra Epee-Bounya, Boston Children's Hospital, boston, MA, United States; Kimberly Goldstein, Boston Children's Hospital, Boston, MA, United States; Rebecca Locke, Harvard Medical School, Boston, MA, United States; Jessica Martin, Boston Children's Hospital, Boston, MA, United States; Gabriela Tew, Boston Children's Hospital, Jamaica Plain, MA, United States; Corinna Rea, Boston Children's Hospital, Boston, MA, United States

Nicole Heredia, Bachelor of Science (she/her/hers)
Clinical Research Assistant II
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Postpartum depression (PPD), spanning mild to severe symptoms, impacts maternal and infant health when untreated. Universal screening and follow-up are crucial for identifying maternal depression and connecting mothers to support.
Objective: This study aimed to establish baseline PPD screening rates at well-child visits, assess follow-up processes, and set a foundation for quality improvement.
Design/Methods: A retrospective, cross-sectional study in two urban pediatric clinics reviewed Edinburgh Postnatal Depression Scale (EPDS) screenings from December 2022 to May 2024 for children aged 2-7 months. An equity analysis was conducted using bivariate and multivariate logistic regression to examine associations between screening completion and race/ethnicity, insurance, and language. Follow-up rates were assessed through provider and social work documentation in patients' charts.
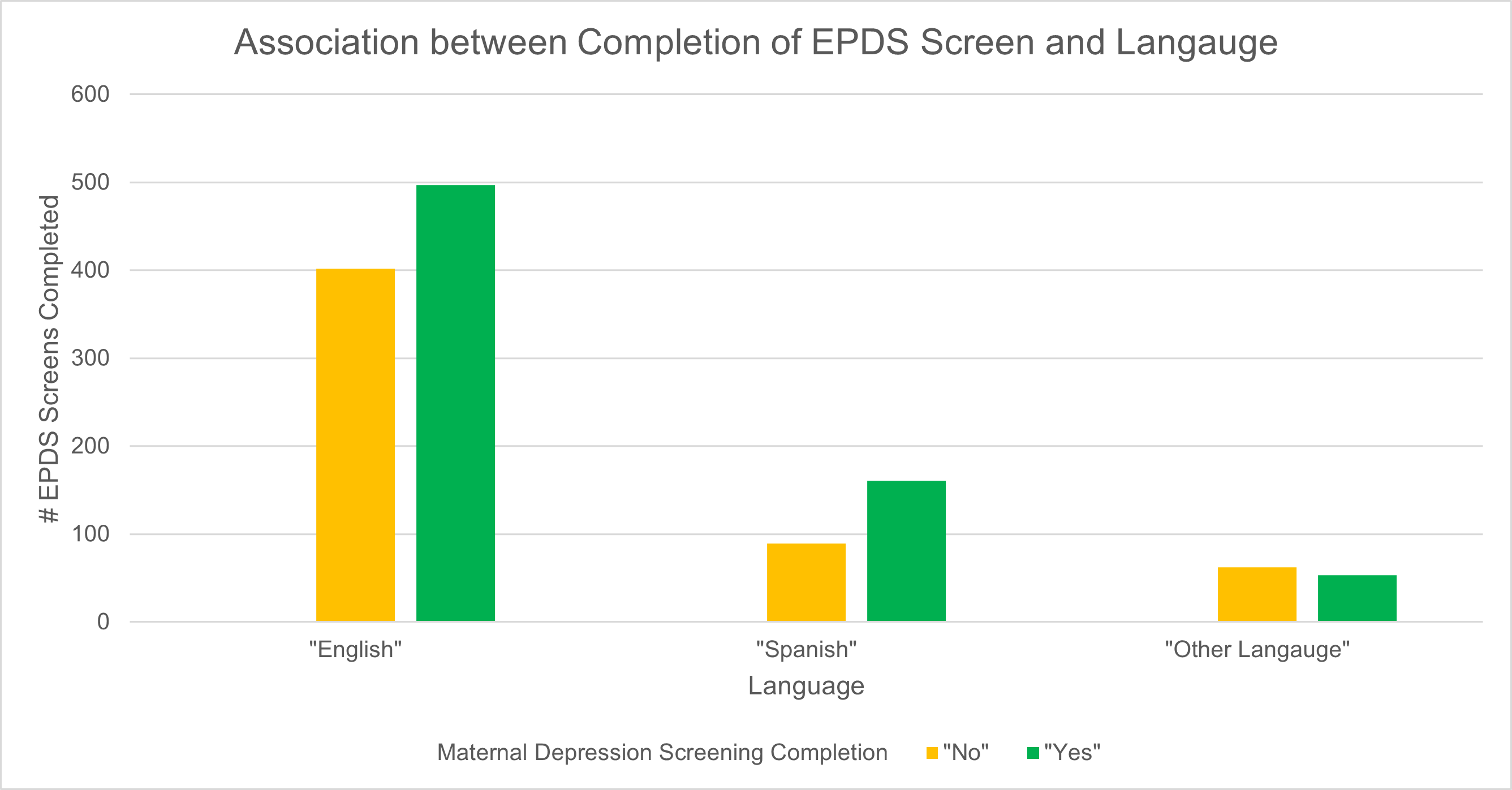
Results: Among mothers attending 2- or 4-month well-child visits (N=2,701), 52.08% were screened for PPD. Including the 6-month visit, 78.37% were screened at least once by 7 months, but only 45.09% were screened twice. In bivariate analysis, language and race/ethnicity were associated with screening completion. 'White, non-Hispanic' mothers had higher odds of screening completion than 'Other Race, non-Hispanic' mothers (OR = 1.39, 95% CI [1.05, 1.85], p = .021). Spanish-speaking mothers had higher odds than English-speaking mothers (OR = 1.69, 95% CI [1.24, 2.31], p < .001), while other-language speakers had lower odds, although not significant (OR = 0.71, 95% CI [0.48, 1.06], p = .090). Insurance type was not significant. In the multivariate model, Spanish-speaking mothers remained more likely to complete screening than English-speaking mothers (OR = 1.51, 95% CI [1.12, 2.02], p = .007), while other-language speakers continued to show lower odds (OR = 0.71, 95% CI [0.48, 1.05], p = .083). Race/ethnicity was no longer significantly different after adjustment. Immediate response rates were 95.41%, but only 47.41% had documented follow-up of service receipt within 90 days, and 9.81% within 45 days. Additionally, 49.29% of mothers who screened positive for PPD reported other social needs, like housing or food insecurity.
Conclusion(s): Immediate response rates were high, but screening rates were lower than expected, with significant language-based disparities and follow-up gaps. Future steps include quality improvement initiatives to enhance screening, provider training, social needs analysis, and cross-cultural insights to foster equitable care.
Follow-up response rates after positive EPDS screens
.png) Immediate response rate is high; follow-up rates at 45 and 90 days show a decrease.
Immediate response rate is high; follow-up rates at 45 and 90 days show a decrease.EPDS screening completion by language
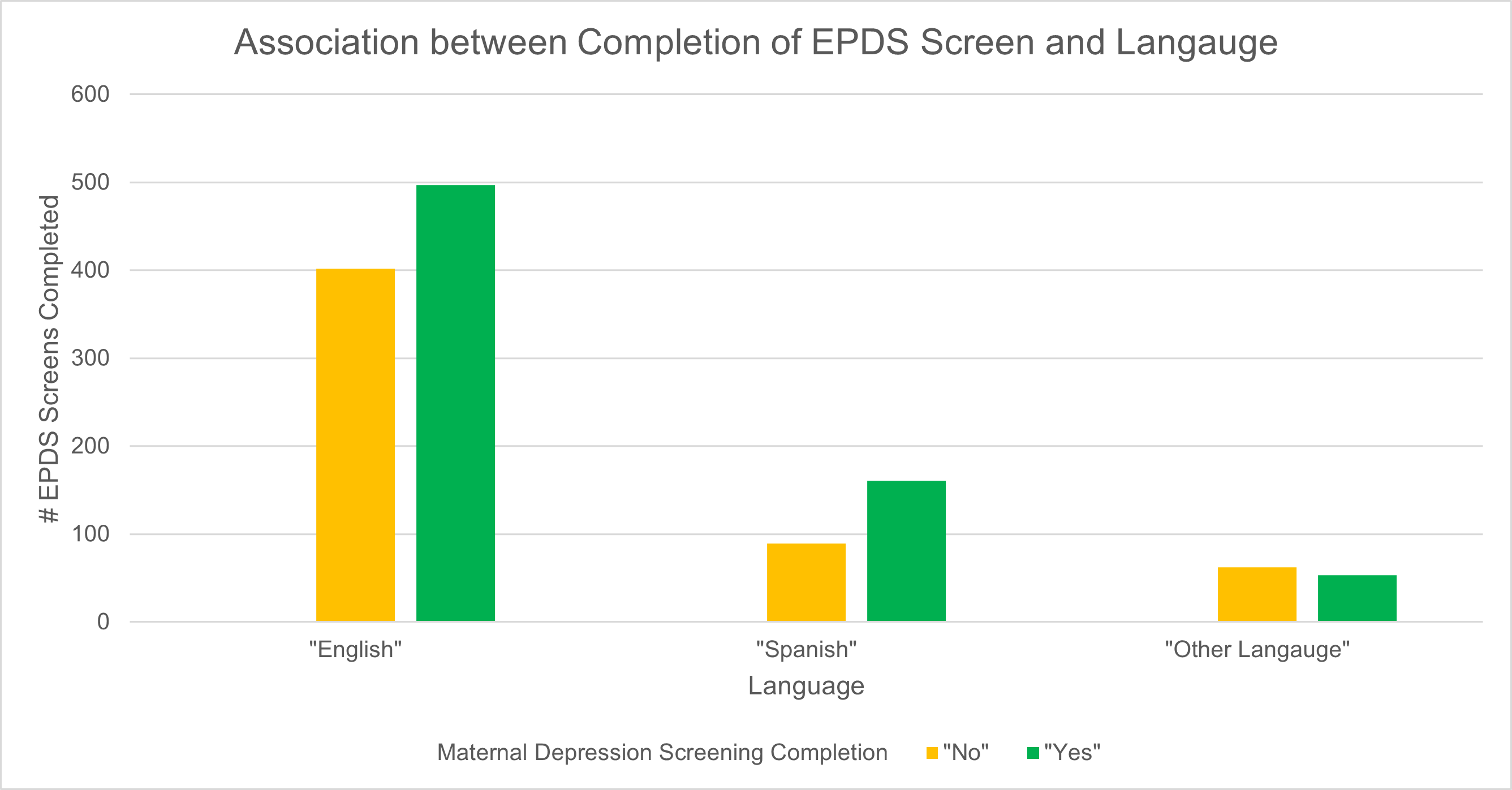 Screening completion rates for EPDS vary by language, with higher completion among Spanish-speaking mothers.
Screening completion rates for EPDS vary by language, with higher completion among Spanish-speaking mothers.Follow-up response rates after positive EPDS screens
.png) Immediate response rate is high; follow-up rates at 45 and 90 days show a decrease.
Immediate response rate is high; follow-up rates at 45 and 90 days show a decrease.EPDS screening completion by language
 Screening completion rates for EPDS vary by language, with higher completion among Spanish-speaking mothers.
Screening completion rates for EPDS vary by language, with higher completion among Spanish-speaking mothers.
