Quality Improvement/Patient Safety 2
Session: Quality Improvement/Patient Safety 2
020 - Fluoride in OU Pediatrics Clinics: Tackling The Most Common Chronic Disease of Childhood in the US.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 20.4578
Kelly Erickson, Oklahoma Childrens Hospital at OU Health, Oklahoma City, OK, United States; Emily De Hoog, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Jill Warren, University of Oklahoma, EDMOND, OK, United States
- KE
Kelly Erickson, MD (she/her/hers)
Resident PGY 3
Oklahoma Childrens Hospital at OU Health
Oklahoma City, Oklahoma, United States
Presenting Author(s)
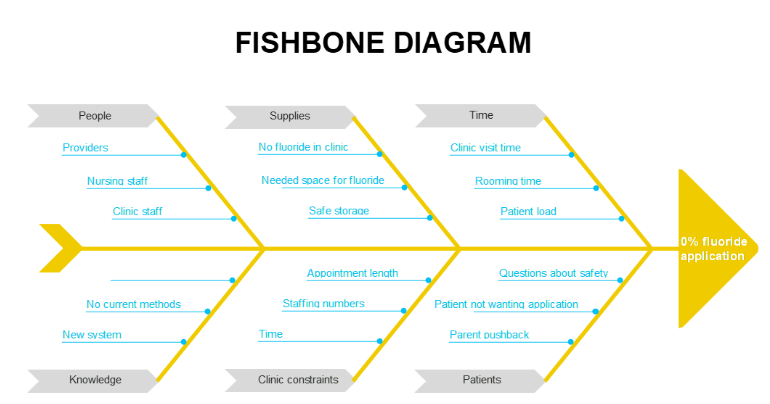
Background: Dental caries, the most common chronic disease among US children, affect 23% of those aged 2-5 and are a major risk factor for adult dental issues. This condition negatively impacts health outcomes, education, and incurs significant costs. The USPSTF recommends applying fluoride varnish to infants and children starting at tooth eruption. However, at OU Primary Care pediatrics clinics, specifically Sooner Pediatrics (SP) and Sooner Pediatrics North (SPN), the fluoride varnish application rate was 0%. Additionally, the clinics lost $6000 in potential revenue for 381 well-child visits in May for children aged 6 months to 5 years.
Objective: Our goal is to increase the fluoride varnish application rate for Medicaid or SoonerCare patients at OU pediatrics clinics from 0% to 60% by June 2024.
Design/Methods: We implemented several PDSA (Plan-Do-Study-Act) cycles. The first intervention made fluoride varnish available and engaged stakeholders to develop an efficient workflow. Surveys assessed team members' perceptions, guiding further improvements. We posted flyers, sent check-in emails, and provided lunch incentives to reach a 40% application goal by January. Fluoride care gaps were identified in Epic but underutilized. We tracked claims data for CPT code 99188 during well-child visits from 6 months to 5 years, excluding 9-month and 15-month visits.
Results: Data collected from the Oklahoma health authority on fluoride varnish applications billed to Medicaid/SoonerCare revealed an initial 0% application rate (August). After PDSA cycle 1 (October-December), SP increased by 49%, and SPN by 44%. By cycle 2 (January-February), both clinics reached 55%. In cycle 3 (March-June), SP recorded 52%, while OU clinics overall achieved 55%. However, SPN’s data was less reliable due to a location change in May.
Conclusion(s): We did not reach 60%, but did improve rates from 0% to 55%. The largest delta followed PDSA 1. This initial success showed the importance of involving team members when building a new workflow. Rising success rates can be attributed to the following two PDSA cycles involving change based on surveys. This worked two-fold, both giving stakeholders the chance to help tweak the new system, but also as a reminder of the new practice. Making it user-friendly and easy to remember was crucial. Reminder emails, care gaps, and a standardized schedule were helpful tools. This success can be used in future QI projects when implementing new clinic workflow. The financial benefit had promising results. The overall loss in revenue for all OU clinics went from $16 to $10 per well child visit from 6mo – 5yrs.
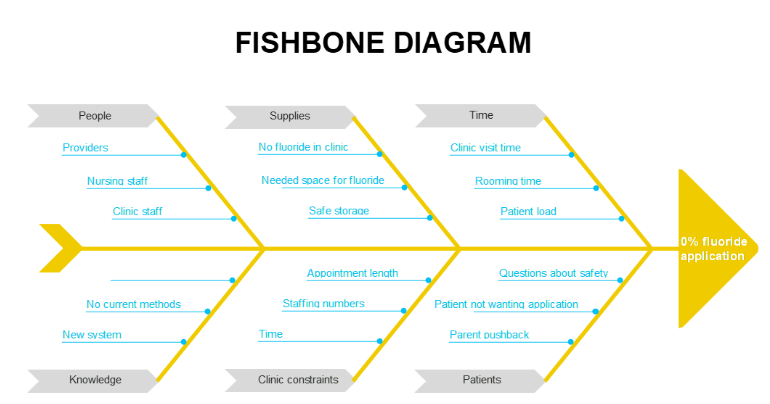
Fishbone diagram
Graph 1: Fluoride varnish rate over time
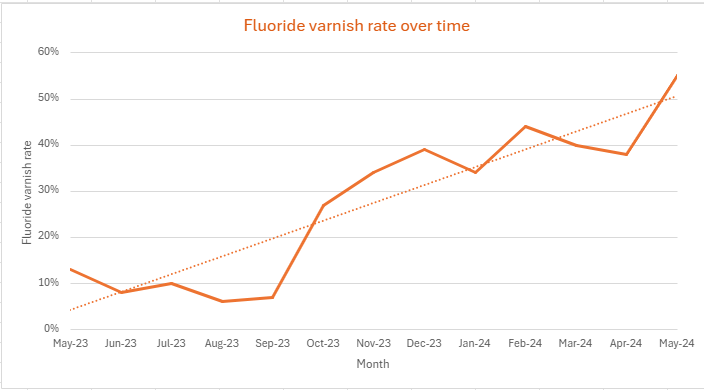
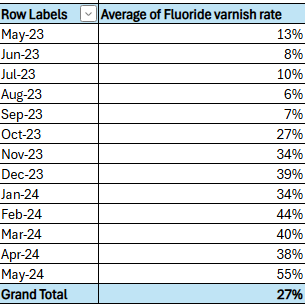
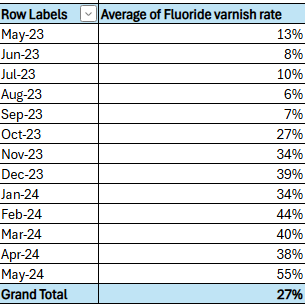
Table 1: Fluoride varnish rate over time
Fishbone diagram
Graph 1: Fluoride varnish rate over time
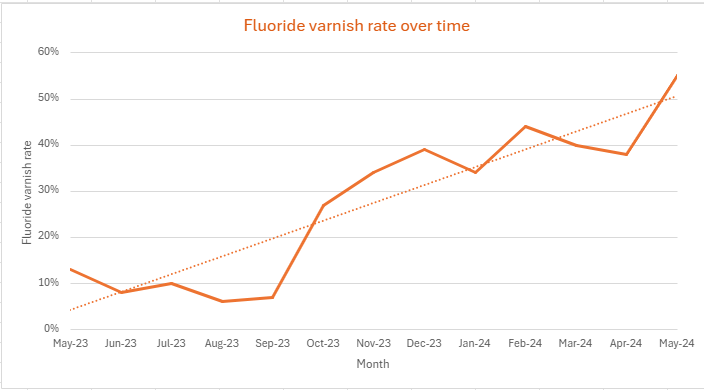
Table 1: Fluoride varnish rate over time