Neo-Perinatal Health Care Delivery: Practices and Procedures 2
Session: Neo-Perinatal Health Care Delivery: Practices and Procedures 2
468 - Cue-Based Oral Feeding Progression Achieves Early Oral Feeding in Extremely Premature Infant
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 468.4261
Mariana Santo, University of Florida Jacksonville, Jacksonville, FL, United States; P Sireesha. Nandula, University of Florida College of Medicine, Jacksonville, FL, United States; Vasantha HS. Kumar, University of Florida College of Medicine, Jacksonville, Jacksonville, FL, United States; Shiva Gautam, University of Florida College of Medicine, Jacksonville, FL, United States; Sanket D. Shah, University of Florida College of Medicine, Jackonsville, FL, United States
- MD
Mariana Diaz, DO (she/her/hers)
Resident
University of Florida Jacksonville
Jacksonville, Florida, United States
Presenting Author(s)
Background: Initiating oral feeding in Extremely Premature Infants (EPI, < 28 weeks gestational age) is a significant milestone for caregivers and parents. However, these infants are often at risk of oral feeding difficulties due to decreased muscle tone and endurance. Neonatal morbidities such as intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), and sepsis can worsen these challenges, leading to longer lengths of stay (LOS). Cue-based oral feeding progression (CB-OFP) involves behavioral assessment and systematic evaluation by speech therapists. In contrast, volume-based oral feeding progression (VB-OFP) focuses on the infant's ability to achieve a predetermined oral feeding volume. There is a paucity of studies regarding better OFP in EPI. We conducted a study to compare the effectiveness of cue-based and volume-based OFP in EPI.
Objective: To assess feeding and discharge metrics of infants achieving full oral feedings using cue-based and volume-based oral feeding approaches in extremely premature infants.
Design/Methods: We retrospectively analyzed premature infants admitted to NICUs at the University of Florida Health (UFH) and Wolfson Children’s Hospital (WCH) from 07/01/2022 to 04/30/2024. A pre-defined OFP protocol was followed at both hospitals, with UFH using a CB-OFP approach and WCH using a VB-OFP approach. Data was analyzed with parametric and non-parametric tests as appropriate. Quantile regression was used to examine the association between OFP and postmenstrual age (PMA) at full oral feeds, adjusting for IVH, NEC, and bronchopulmonary dysplasia (BPD).
Results: Of the 134 eligible infants, 63 followed the CB-OFP protocol, and 71 followed the VB-OFP protocol (Figure 1). Infants in the CB-OFP cohort were SGA and had fewer morbidities, such as IVH, NEC, and BPD (Table 1). Feeding characteristics in both groups are shown in Table 2. Oral motor stimulation was initiated early, leading to the early start of oral feeding in CB-OFP compared to VB-OFP infants (34.5 vs 36 weeks, p = 0.0006). Infants in CB-OFP also required fewer days to achieve full oral feeding. PMA at full oral feeding (p = 0.0001) and length of stay (p = 0.003) were significantly lower in CB-OFP infants.
Conclusion(s): Early oral motor stimulation and initiation of oral feeding were associated with reduced LOS and earlier achievement of full oral feeding in EPI. The cue-based oral feeding approach has substantial benefits compared to volume-based feeding in extremely premature infants. Future studies should address the benefits of CB-OFP on maternal-infant bonding and the promotion of breastfeeding in these infants.
Table 1: Comparison of Cue-based feeding and volume-based feeding
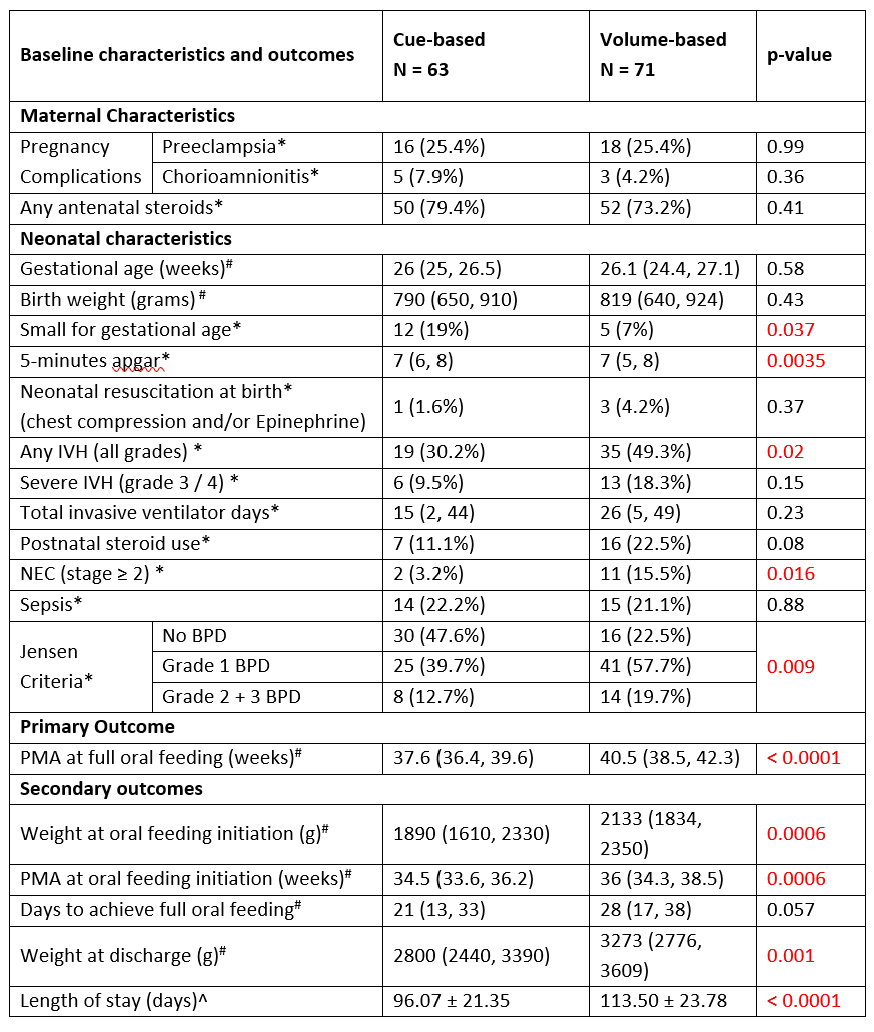 * Counts (percentages), # median (quartile range), ^ mean ± standard deviation
* Counts (percentages), # median (quartile range), ^ mean ± standard deviationBPD; Bronchopulmonary dysplasia, IVH; intraventricular hemorrhage, NEC; necrotizing enterocolitis, PMA; postmenstrual age
Table 2: Multivariable analysis on feeding data
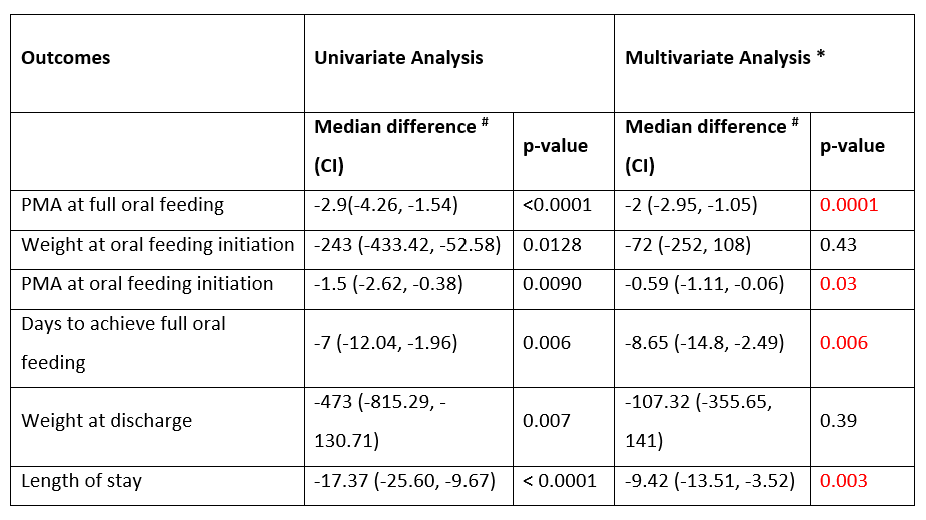 *Analysis adjusted for SGA, NEC, IVH and BPD
*Analysis adjusted for SGA, NEC, IVH and BPD# Difference of median between two groups and compared via quantile regression
SGA; Small for gestational age, BPD; Bronchopulmonary dysplasia, IVH; intraventricular hemorrhage, NEC; necrotizing enterocolitis, PMA; postmenstrual age
Figure 1: Comparison of two oral feeding progression protocol
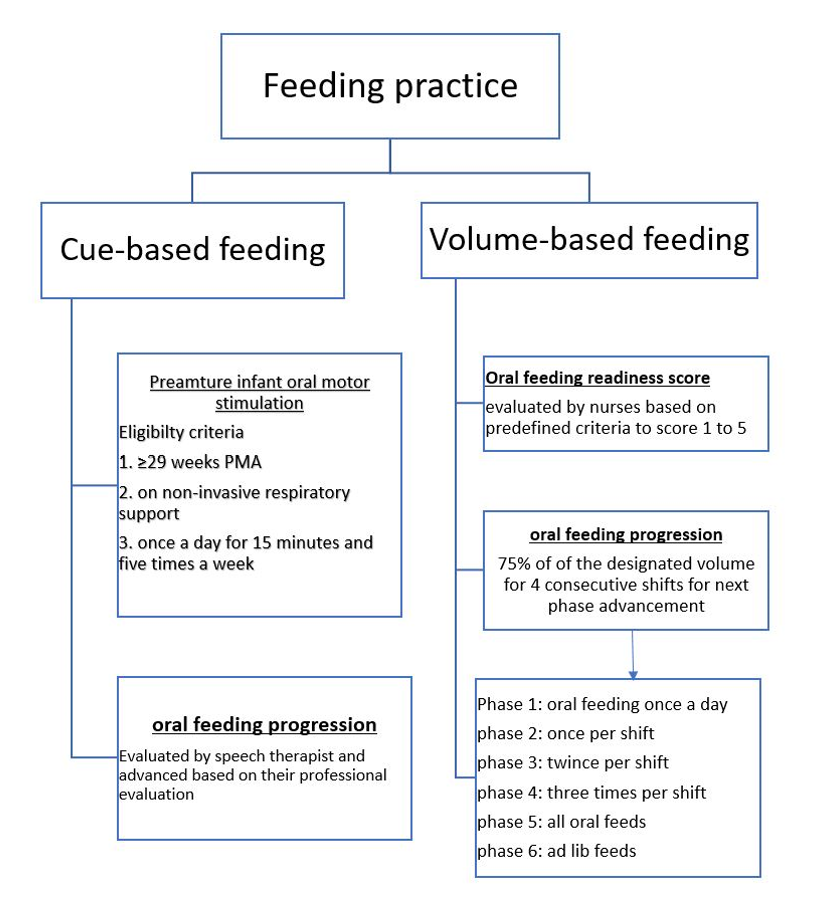 PMA; postmenstrual age
PMA; postmenstrual age
