Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
057 - Implementation of Delivery Room Echocardiography for Neonates with d-Transposition of the Great Arteries
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 57.5285
Emma Harding, University of Colorado School of Medicine, Denver, CO, United States; Blair Weikel, University of Colorado School of Medicine, Aurora, CO, United States; Theresa Grover, University of Colorado School of Medicine, Aurora, CO, United States; Jeanne Zenge, University of Colorado School of Medicine, Aurora, CO, United States; Regina M. Reynolds, Children's Hospital Colorado, Denver, CO, United States; Rebecca Shay, University of Colorado School of Medicine, Aurora, CO, United States

Emma Harding, MD (she/her/hers)
Fellow
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Neonates with dextro-transposition of the great arteries (d-TGA) are at risk for hemodynamic instability and need for urgent balloon atrial septostomy (BAS); current fetal echocardiographic findings have good specificity but poor sensitivity for predicting postnatal decompensation.
Objective: Our institution’s fetal care center offers collaborative prenatal counseling and delivery planning for infants with cardiac defects. To improve care for d-TGA patients, in-delivery room echocardiogram with interpretation by a cardiologist was standardized for all infants in September 2022, regardless of the degree of prenatal concern for atrial level restriction. The primary aim of this retrospective analysis was to compare timing of first postnatal echocardiogram in pre-intervention and intervention cohorts. The secondary aim of this review was to compare timing of BAS, if indicated, in these two groups.
Design/Methods: This study was performed at our children’s hospital with a level IV neonatal intensive care unit (NICU) and cardiac intensive care unit (CICU). A retrospective chart review was performed for infants with d-TGA born between January 2020-August 2023. We compared the populations before and after in-delivery room echocardiogram was standardized for all infants with d-TGA. We also used control charts to track response to our interventions over time.
Results: We studied a total of 24 infants with d-TGA with 14 in the pre-intervention period and 10 in the intervention period. Both cohorts had similar prenatal echocardiograms with 93% and 90% appearing unrestrictive at the atrial level in the pre- and intervention periods, respectively. The time to echo improved from a median of 130.5 minutes of life to a median of 6 minutes of life and there was less variability during the intervention period (p < 0.0001). Additionally, a similar percentage of infants underwent BAS in both groups (57% and 60%), but the time to procedure was reduced by nearly 50% (median of 221 minutes vs. 115.5 minutes).
Conclusion(s): Standardizing in-delivery room echocardiography with cardiology interpretation for all infants with d-TGA improved time to echocardiogram and ultimately time to BAS, if needed. Upcoming steps in our study are to collaborate with the fetal cardiology team to further investigate level of prenatal concern and presence of postnatal instability or need for BAS. We plan to develop additional quality improvement initiatives to continue optimizing resource utilization and to create cardiac lesion-specific guidelines to aid with delivery room management for newborns with complex cardiac disease.
Table 1
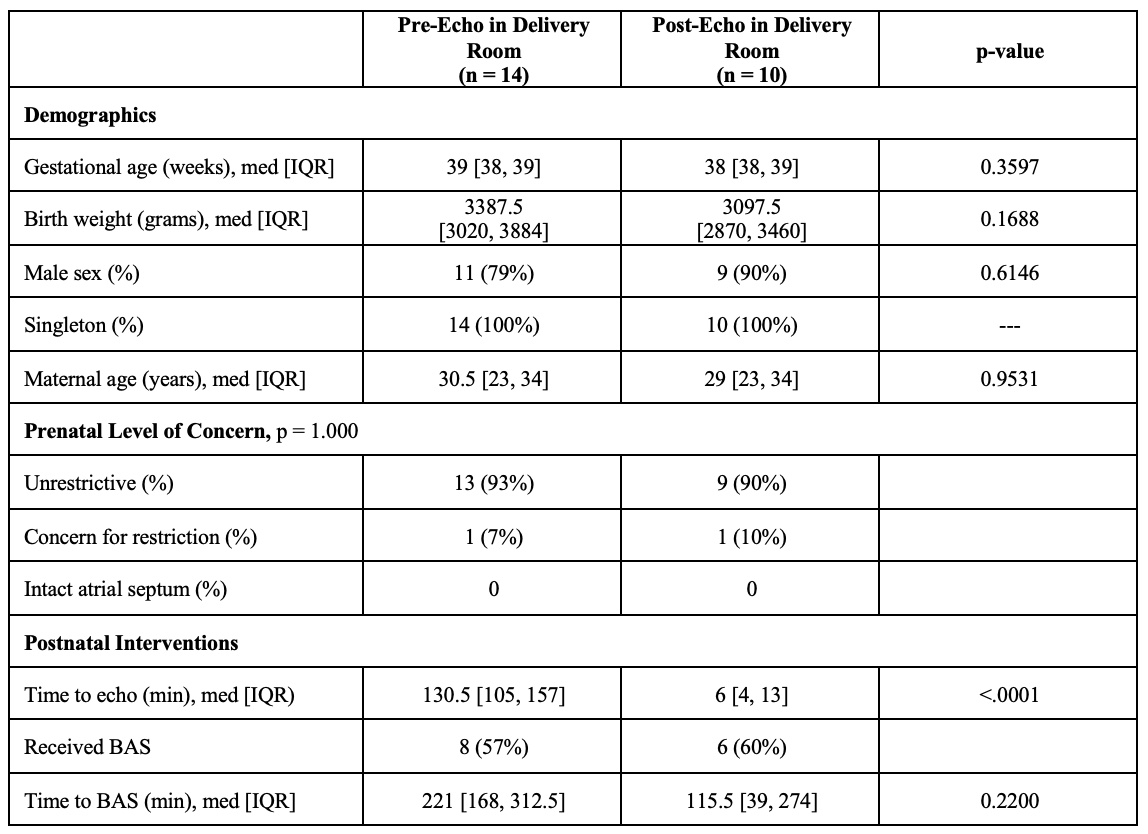
Figure 1
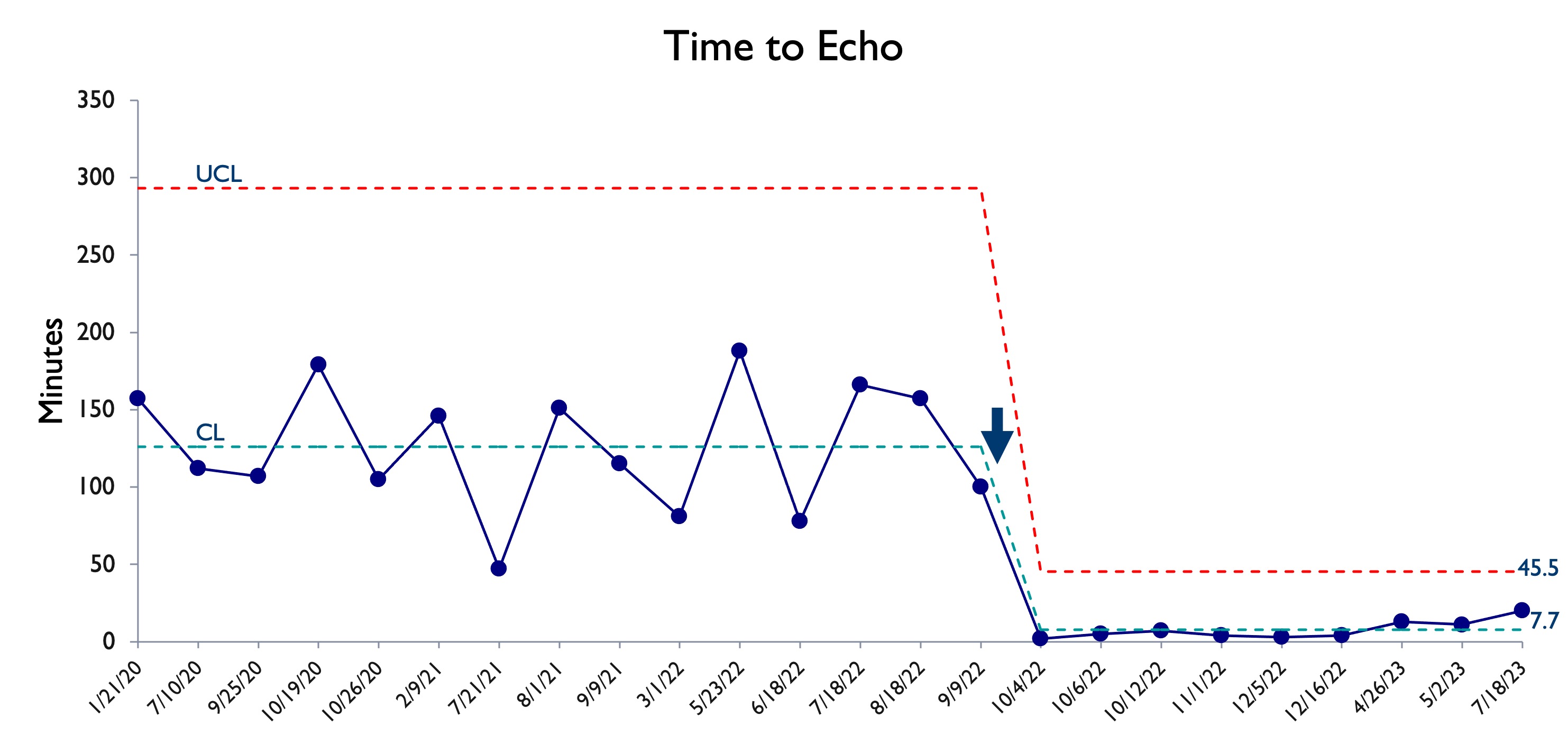 Control chart of time to first postnatal echo
Control chart of time to first postnatal echoFigure 2
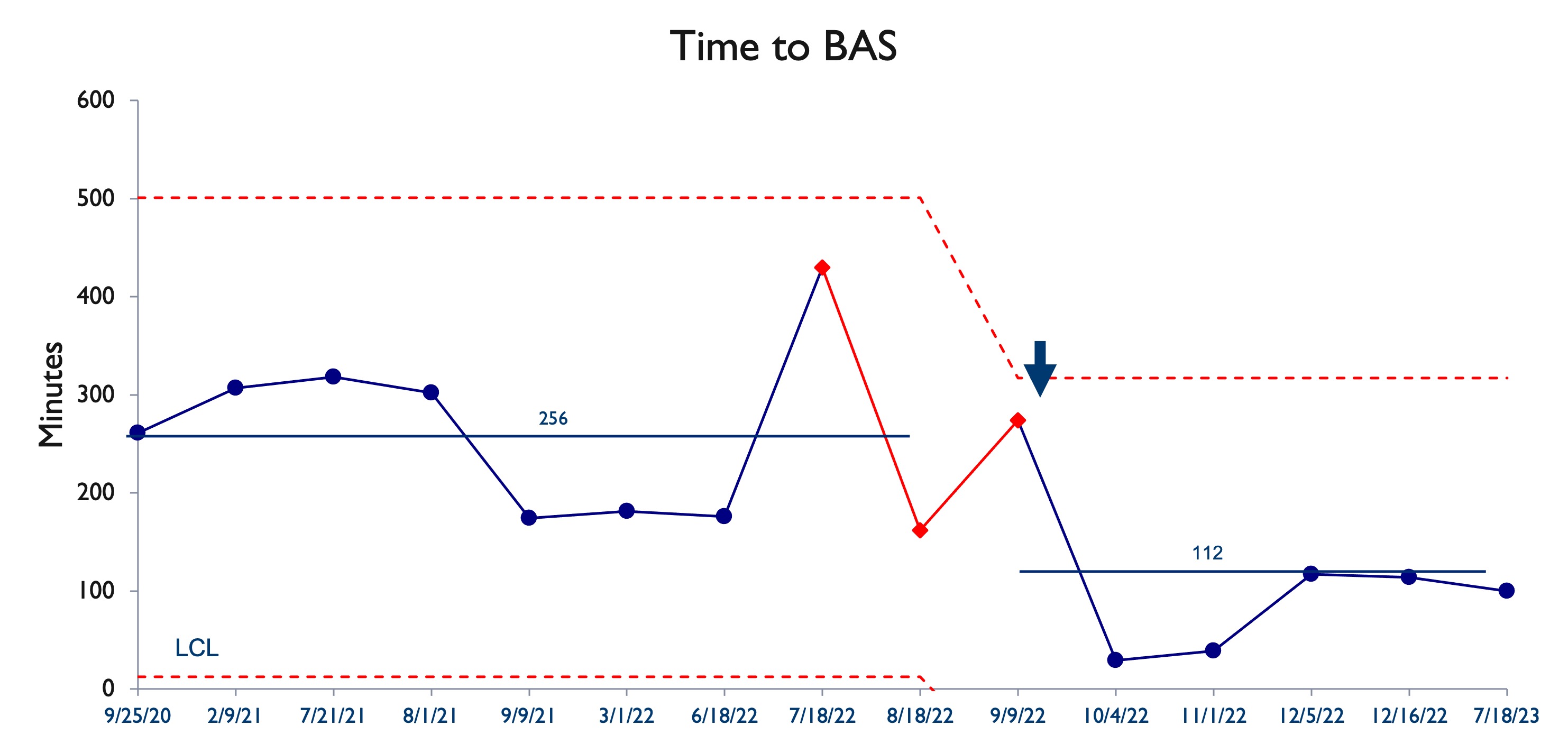 Control chart of time to balloon atrial septostomy
Control chart of time to balloon atrial septostomy

