Critical Care 1
Session: Critical Care 1
112 - Identification and Trends of Adverse Events in Patients Admitted to a Pediatric Critical Care Unit (PCCU)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 112.5255
Devika Singh, Children's Hospital, Vaughan, ON, Canada; Michael Miller, The University of Western Ontario - Schulich School of Medicine & Dentistry, London, ON, Canada; Cory Anderson, The University of Western Ontario - Schulich School of Medicine & Dentistry, London, ON, Canada; Douglas Fraser, The University of Western Ontario - Schulich School of Medicine & Dentistry, London, ON, Canada
Devika Singh, MD, BHSc (she/her/hers)
Pediatric Resident
The University of Western Ontario - Schulich School of Medicine & Dentistry
London, Ontario, Canada
Presenting Author(s)
Background: Pediatric critical care has advanced significantly, improving outcomes for critically ill children but also increasing the risk of adverse events—unintended injuries or complications arising from intensive care. Monitoring systems like the Adverse Event Management System (AEMS) are critical for identifying risks, developing interventions, and enhancing patient safety within Pediatric Critical Care Units (PCCUs). Despite the importance of tracking these incidents, long-term trends remain underexplored, particularly in pediatric care settings.
Objective: The objective of this study was to analyze trends in adverse events reported over a 10-year period in the PCCU, focusing on frequency of events, length of stay, and trends during and after the COVID-19 pandemic.
Design/Methods: This project involved a retrospective analysis of AEMS reports from a PCCU over a 10-year span. Data collected included patient demographics, reasons for admission, length of stay, and adverse event types and severity. Events were classified into categories ranging from near misses to critical incidents based on harm severity. The length of stay (LoS) and number of adverse events were analyzed using ARIMA (auto-regressive, integrated, moving average) interrupted time series models.
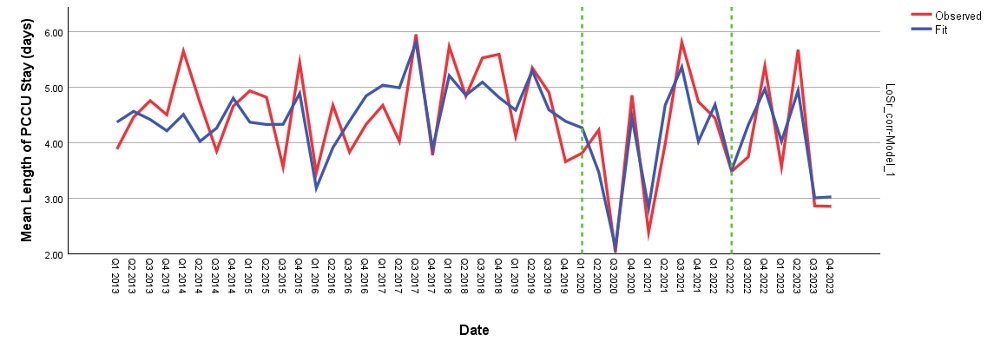
Results: Analyzing adverse events using an interrupted time series model revealed an average rate of 16.11 AEMS per 100 cases, indicating stable conditions prior to the pandemic (Figure 1). Adverse events jumped by 7.32 AEMS per 100 cases at the pandemic's onset (p=0.049), followed by a decrease of 1.71 AEMS per 100 cases for each additional quarter year during the pandemic (p=0.009). In terms of LoS, the average baseline was 4.35 days, with a notable drop of -1.38 days at the start of the pandemic (p < 0.001). This trend was accompanied by a slight increase of 0.11 days per quarter during the pandemic (p=0.021), but post-pandemic results showed no significant change over time (Figure 2). Comprehensive analysis indicates that AEs increased during the pandemic, while LoS exhibited a complex pattern of fluctuation with significant reductions and slight increases over time.
Conclusion(s): This study underscores the importance of continuous monitoring and analysis of adverse events to improve patient safety in PCCUs. Identifying trends in adverse events enables the development of targeted interventions to prevent future incidents and enhance the quality of care. The findings will provide a framework for other institutions to assess their adverse event data, fostering a culture of safety and continuous improvement in pediatric critical care settings.
Figure 1: Trends in Pediatric Adverse Events: An Interrupted Time Series Model Before, During, and After COVID-19
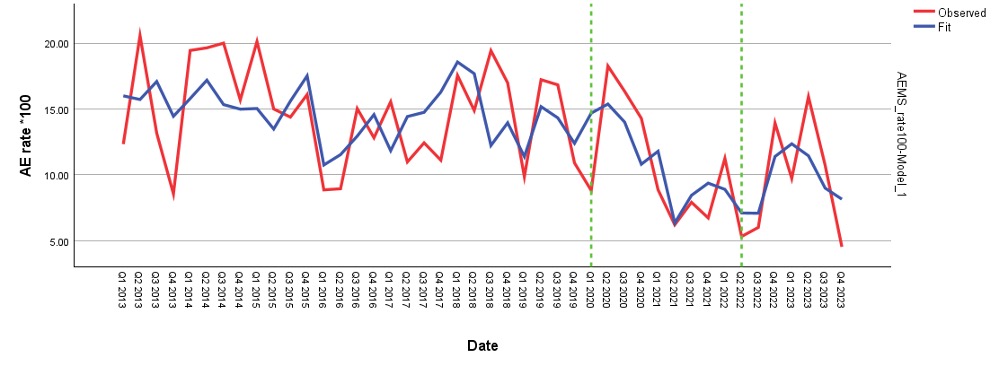
Figure 2: Trends in LoS in Pediatric Patients Before, During, and After COVID-19