General Pediatrics 2
Session: General Pediatrics 2
714 - Implementing a screener for pediatric anxiety for patients aged 8-11 at a federally qualified healthcare center
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 714.5318
Gabrielle E. Sanatani, Children's Hospital Colorado, Denver, CO, United States; Gabby Pantalena, Denver Health, Denver, CO, United States; Rachel Benson, Denver Health and Hospital Authority, Denver, CO, United States; Sara J.. Hills, University of Colorado School of Medicine, Denver, CO, United States; Jessica Jack, Denver Health and Hospital Authority, Denver, CO, United States

Gabrielle E. Sanatani, MB, BCh, BAO (she/her/hers)
Resident
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Anxiety disorders are a common childhood condition, present in up to 20% of youth globally, with earlier age of onset being associated with worse outcomes. In late 2022, the United States Preventive Services Taskforce (USPSTF) recommended expanding screening from ages 11 through 18 to ages 8 through 18 in order to identify and provide early intervention to children suffering from anxiety.
Objective: To implement a validated screening tool to address the USPSTF recommendation to aid in identifying children ages 8 through 11 with anxiety.
Design/Methods: This study took place at a federally qualified healthcare center (FQHC) in Denver, Colorado. The clinic implemented the Screen for Child Anxiety Related Disorders (SCARED) 5-item tool at all visits for patients aged 8 through 11. The tool was utilized at all acute and well child visits for patients who spoke English or Spanish during a six-month period from 11/1/23-4/30/24. A positive screen was considered as a score > 3. Screeners were administered on paper by clerical staff and data were collected manually. Plan-do-study-act (PDSA) cycles were performed on a weekly basis. Demographic data were analyzed using Chi Square or Fishers Exact test. Run charts were used to evaluate the percentage of eligible visits. Outcomes of positive screens were assessed by chart review.
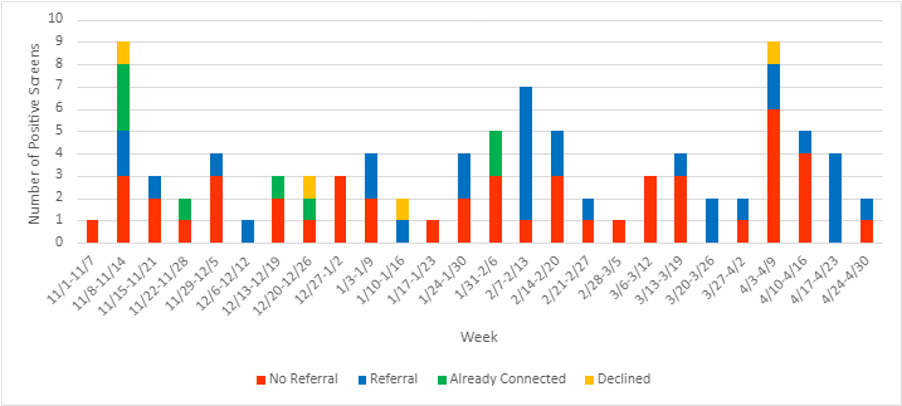
Results: 54.6% (n=277) of eligible patient visits were screened during the six-month period (Table 1). There was a correlation between the chart being marked as an eligible visit for screening and whether patients were screened (Figure 1). Having a screening champion in clinic was the most successful way to increase screening rates. There were no significant demographic differences between those screened and not screened. 33.9% of screened patients were positive for anxiety with 52% being female and there were no significant differences in sex, age, race, ethnicity, or insurance status. The majority of patients who screened positive had no subsequent referral for further intervention with a mental health specialist (Figure 2).
Conclusion(s): This is the first study implementing the updated USPSTF recommendations at a FQHC using the SCARED 5-item tool. This study demonstrated feasibility of implementation of the screening tool with successful identification of patients with anxiety; however, further data are needed to determine if improved screening results in improved mental health outcomes. Following this study, the SCARED screening tool will be integrated into the electronic health record and utilized at all well child visits.
Table 1. Demographic data of screened patients. * Fisher’s exact test.
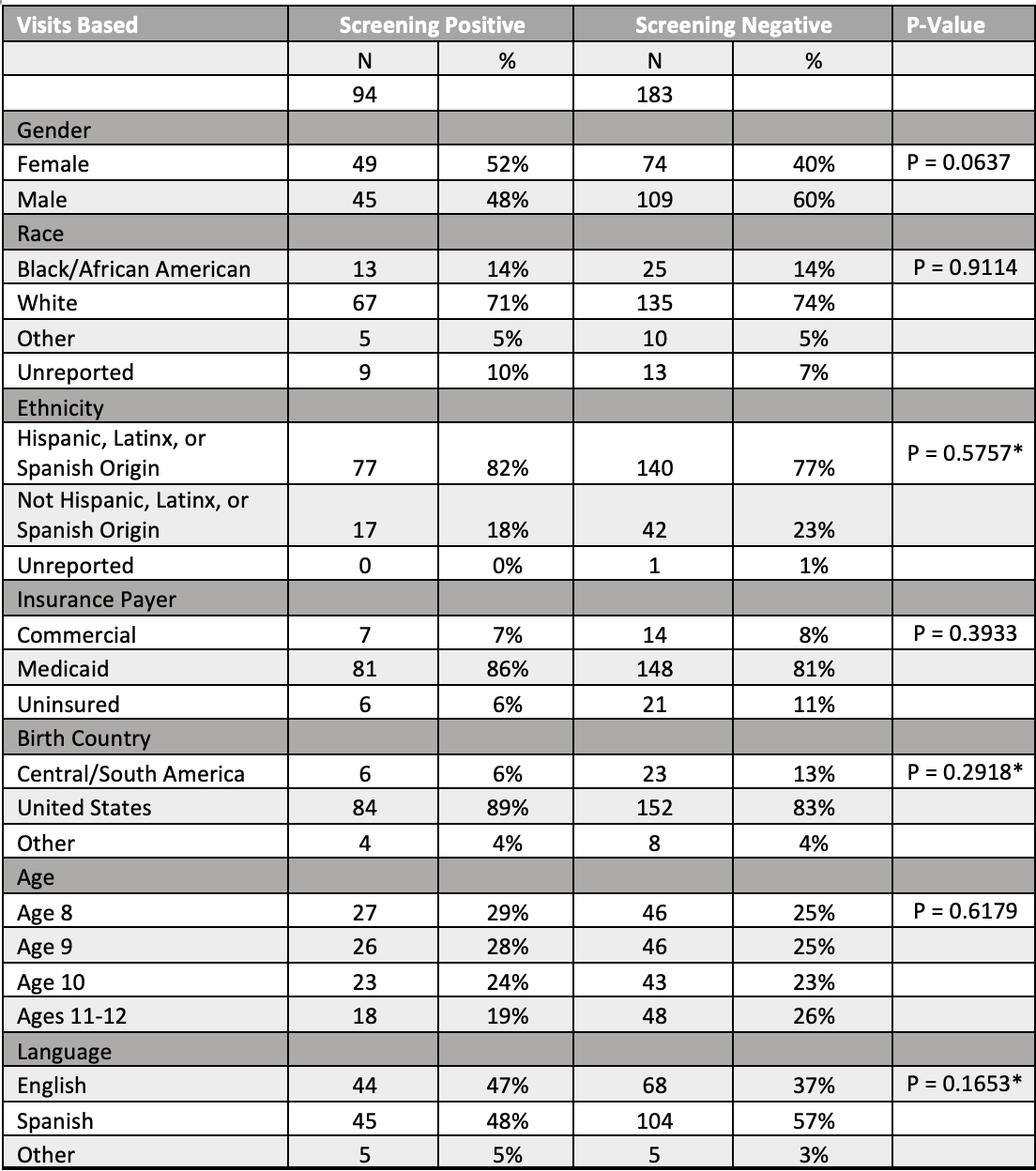
Figure 1: Percentage of visits screened.
.png) 1: Discussion with clerks to improve screening handout at front desk. 2: Screening champion present in clinic daily for entire month. 3: Reminder email sent to clerks and staff. 4: Discussion with clerks, reminder email sent. 5: Reminder email sent, verbal reminders during daily huddle meetings. 6: Screening champion monitoring schedule.
1: Discussion with clerks to improve screening handout at front desk. 2: Screening champion present in clinic daily for entire month. 3: Reminder email sent to clerks and staff. 4: Discussion with clerks, reminder email sent. 5: Reminder email sent, verbal reminders during daily huddle meetings. 6: Screening champion monitoring schedule. Figure 2: Outcomes for patient visits that scored > 3 on SCARED screener