Quality Improvement/Patient Safety 3
Session: Quality Improvement/Patient Safety 3
036 - Improving Resident Participation in Rotation Feedback: A Quality Improvement Initiative
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 36.5293
Sidney JB. Hilker, Boston Children's Hospital, Boston, MA, United States; Michael D. Fishman, Boston Children's Hospital, Boston, MA, United States; Victoria R.. Bradford, Boston Children's Hospital, BOSTON, MA, United States; Christine C. Cheston, BMC Dept of Pediatrics, Boston, MA, United States; Carolyn Marcus, Boston Children's Hospital, Boston, MA, United States; Laura Chiel, Boston Children's Hospital, Boston, MA, United States

Sidney JB Hilker, MD (she/her/hers)
Chief Resident
Boston Children's Hospital
Cambridge, Massachusetts, United States
Presenting Author(s)
Background: Clinical rotation feedback from residents to programs is important for training program improvement, yet resident participation in feedback can be difficult to elicit and sustain. Others have explored barriers to resident self-assessment and programmatic feedback, but interventions to support resident participation in feedback in large residency programs are understudied.
Objective: This quality improvement (QI) study aimed to measure the impact of interventions to overcome program-identified barriers to resident participation in rotation feedback, including: logistical challenges, lack of time, and unclear value of feedback. We aimed to increase the average number of evaluations completed per resident per month from a baseline of 0.19 to 0.50 over 20 months based on the number of residents on rotations with an eligible evaluation.
Design/Methods: This study took place in an urban pediatric residency program including 152 residents across three hospitals and 27 clinical rotations residents between September 2020-May 2023. Participation in clinical rotation feedback was tracked via resident completion of an anonymous six-question, Qualtrics-based evaluation form for each 2-4 week rotations. Plan-Do-Study-Act (PDSA) cycles were implemented, and statistical process control charts were used to identify special cause variation for our primary outcome: feedback completion rate. PDSA cycles focused on improving (1) evaluation tracking, (2) transparency, and (3) individualized completion feedback (Figure 1).
Results: After three PDSA cycles, participation increased from an average 0.19 to 0.4 evaluations per resident per month (Figure 2). Sending residents personalized reminder emails using an automated system had the largest impact on participation with a peak participation of 0.7 evaluations per resident in one month.
Conclusion(s): Interventions to personalize the evaluation process and reduce logistical barriers through individualized reminders had the largest impact on resident participation in rotation feedback. Future studies are needed to understand the sustainability of interventions and the impact on quality.
PDSA Interventions
.png) Interventions, date of implementation and result organized by primary driver and PDSA cycle..
Interventions, date of implementation and result organized by primary driver and PDSA cycle..Evaluations Complete per Resident by Month
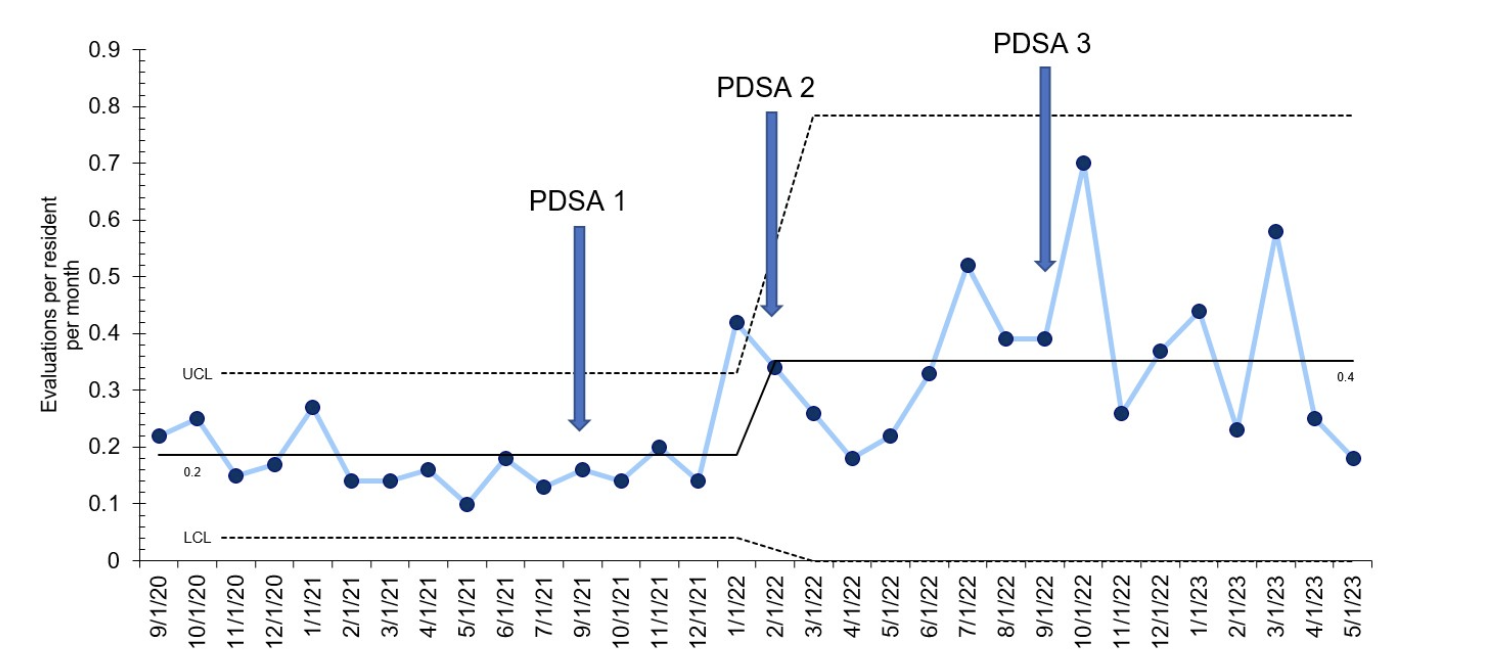 Individual Control Chart for primary outcome: number of evaluations per resident per month
Individual Control Chart for primary outcome: number of evaluations per resident per month

