Medical Education 1: Curricular innovations and assessment 1
Session: Medical Education 1: Curricular innovations and assessment 1
486 - Efficacy of a “Training-the-Trainer” Model for Mentors to Support Pediatric Emergency Care Coordinators: A Retrospective Multi-State Study
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 486.5080
Cage T. Cochran, Yale School of Medicine, New Haven, CT, United States; Sally K.. Snow, self employed, Graham, TX, United States; Camilia Brandt, Improving Pediatric Acute Care Through Simulation, Fenton, MI, United States; Erin Montgomery, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin Michaels, Improving Pediatric Acute Care Through Simulation (ImPACTS), Guilderland, NY, United States; Elizabeth Sanseau, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Sofia Grigoria Athanasopoulou, Yale School of Medicine, New Haven, CT, United States; Marc Auerbach, Yale School of Medicine, new haven, CT, United States

Cage T. Cochran (he/him/his)
Research Associate
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Low Pediatric Readiness scores in Emergency Departments (EDs) is associated with decreased survival among children receiving emergency care; however, many EDs lack the necessary resources and training to improve their scores. A “Train-the-Trainer” program was used to train a large workforce of nurse mentors from TX and MI to establish, train, and assist Pediatric Emergency Care Coordinators (PECCs) in local EDs. A retrospective pre-post quantitative study was used to evaluate the success of the program in training regional mentors.
Objective: To evaluate the success of a Train the Trainer program in training regional nurse mentors
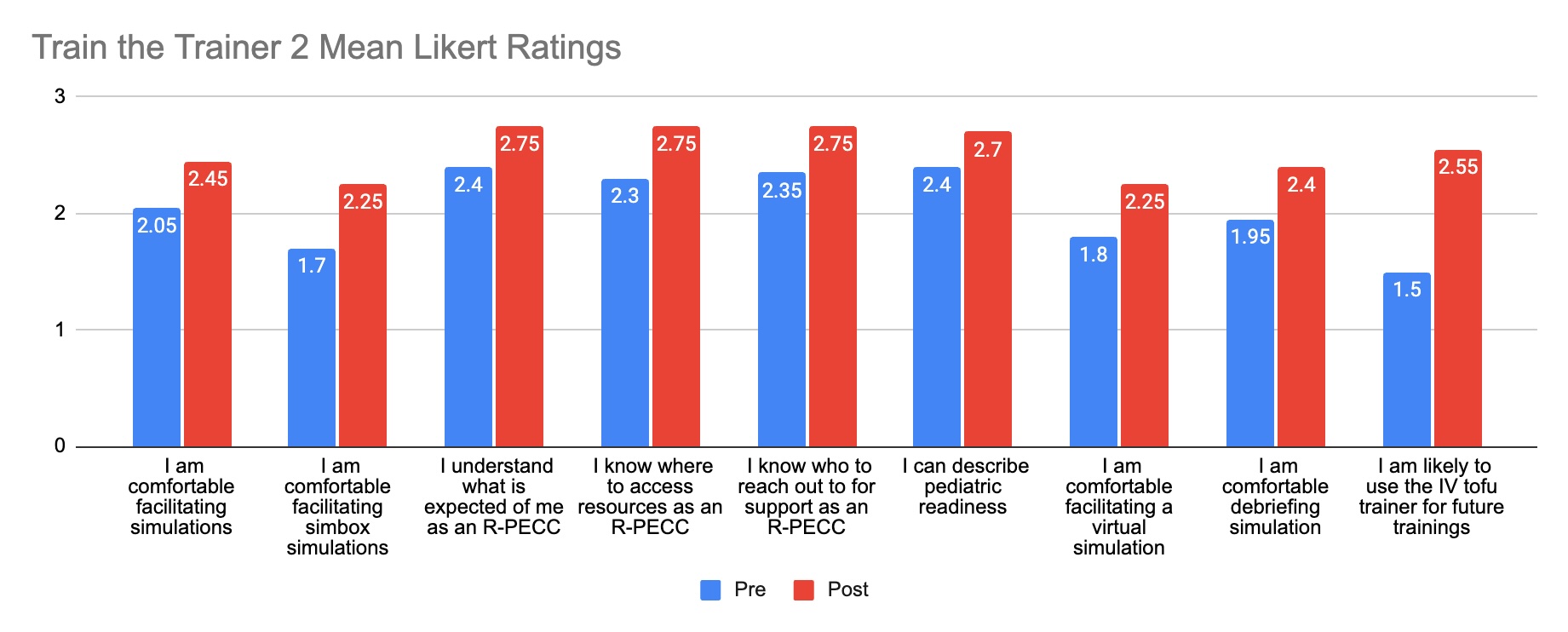
Design/Methods: Mentors were trained in simulation-based pediatric readiness improvement with two “Train the Trainer” sessions over three months. The first training was an in-person one-day session, and the second training was a hybrid one-day session that occurred three months later. The first session was designed to orient the mentors to their role, familiarize them with pediatric readiness, and build their confidence in facilitating simulations (sims). The second session was designed to reinforce the curriculum from the first session while introducing new resources and building mentor confidence in simulation debriefing. Following each training session, participants were given a quantitative survey using a 3-point Likert scale to assess their perceived knowledge and confidence gained.
Results: Thirty nurses participated in the first session, and 20 returned for the second. Net promoter scores were high for both sessions at 73.3 and 55 respectively. Before the first session, 90% of participants felt comfortable facilitating simulations, but only 40% felt comfortable facilitating SimBox simulations. Following the session, these percentages increased to 100% and 96.7% respectively. Mean Likert ratings for all questions increased after the first round. The second session saw an increase in the percentage of participants entering comfortable facilitating SimBox (+25%), knowledgeable about the mentor role (+28.3%), and understanding pediatric readiness improvement (+13.3%). After the second session, mean likert ratings for all questions increased, with understanding of new resources having the largest change (+1.05).
Conclusion(s): The “Train the Trainer” model successfully prepared a large workforce of regional mentors to train PECCs in community EDs across TX and MI by building confidence in sim facilitation and improving knowledge in pediatric readiness. The model holds potential for the expansion of simulation-based pediatric readiness improvement across a diverse range of EDs.
Mean Likert Ratings for Train the Trainer #1
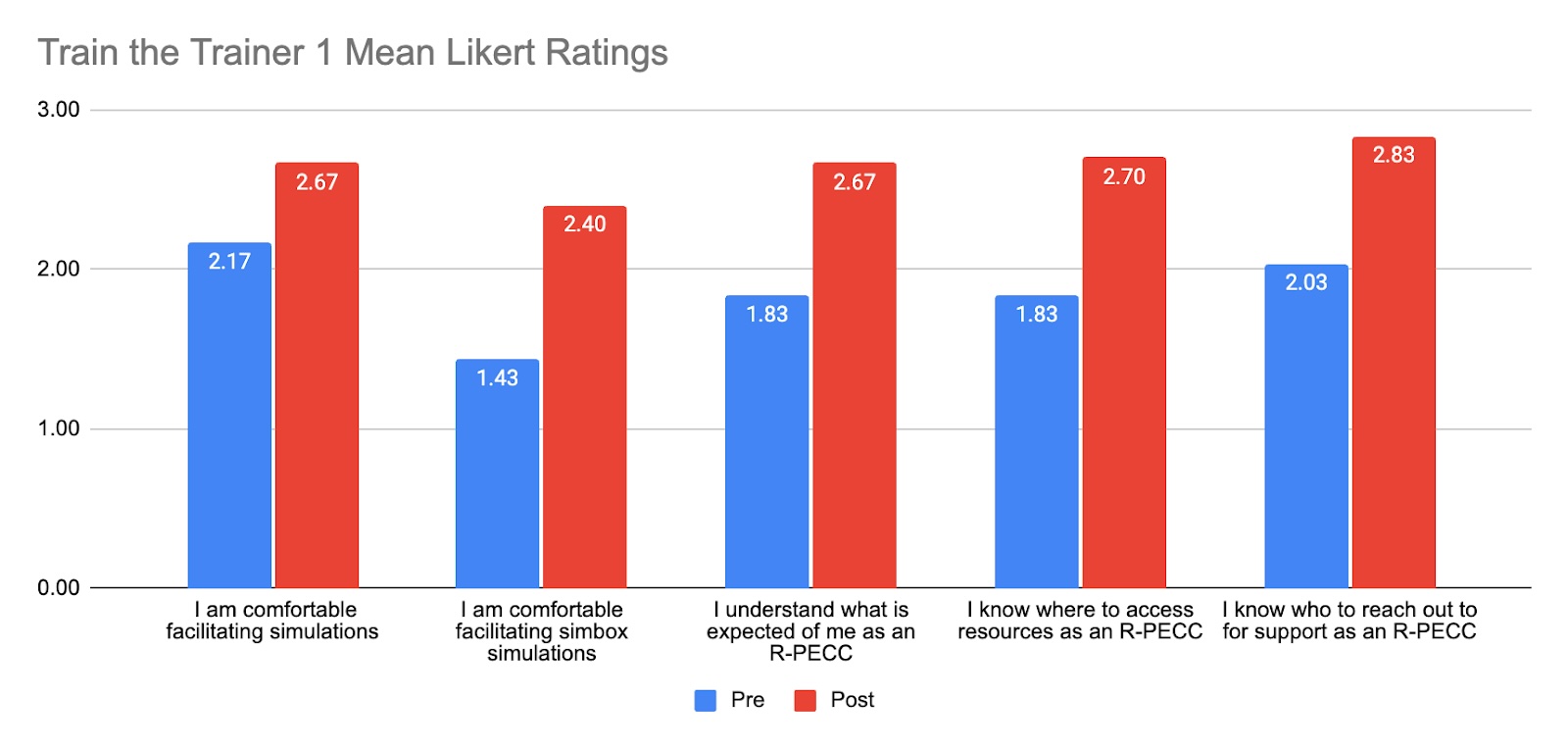
Mean Likert Ratings for Train the Trainer #2