Neonatal Hemodynamics and Cardiovascular Medicine 1
Session: Neonatal Hemodynamics and Cardiovascular Medicine 1
192 - Efficacy and Safety of Transcatheter PDA Closure in Extreme Low Birth Weight Infants on High-Frequency Ventilation
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 192.5031
Omar Abu Anza, UC Davis Children's Hospital, Sacramento, CA, United States; Yogen Singh, UC Davis Children’s Hospital, Sacramento, CA, United States; Frank F.. Ing, University of California Davis Children's Hospital, Sacramento, CA, United States
- OA
Omar Abu Anza, MD
Fellow
UC Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background: Hemodynamically significant patent ductus arteriosus (hsPDA) in very low birth weight (VLBW) infants is often associated with hemodynamic instability requiring significant respiratory support. Infants requiring high-frequency ventilation (HFV) pose additional challenges.
Objective: We aim to assess the safety & efficacy of transcatheter (TC) PDA closure in this high-risk cohort.
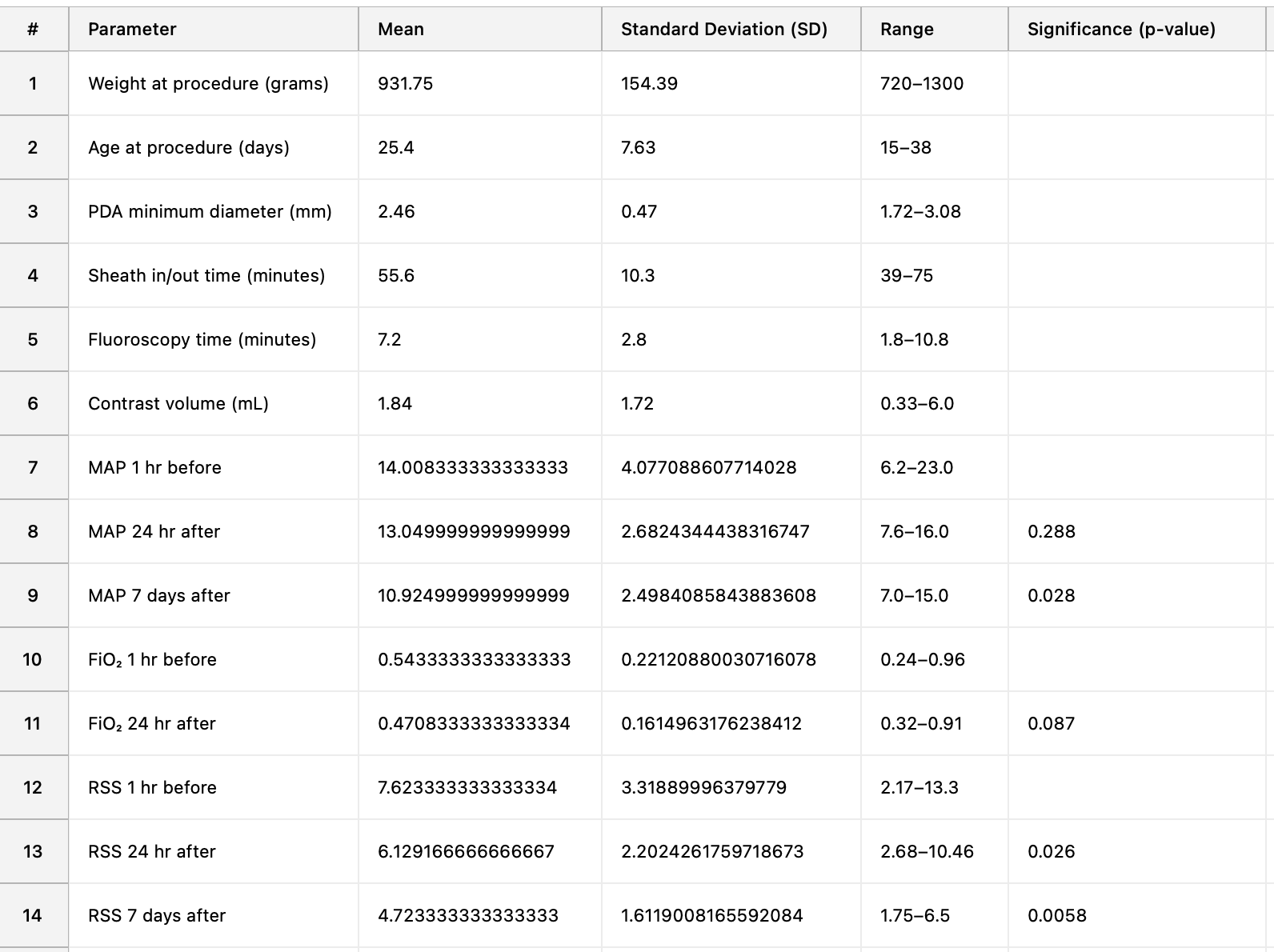
Design/Methods: All VLBW infants who underwent TC PDA closure from 1/2019 to 10/2024 while on HFV were analyzed. Patient profile included gestational age (GA), age & weight at PDA occlusion & other comorbidities. Procedural data included PDA diameter, procedure & fluoroscopy time, and contrast used. Outcome metrics included successful PDA occlusion, and adverse events (post-ligation syndrome (PLS), tricuspid regurgitation (TR), flow obstruction). Respiratory parameters (mean airway pressure (MAP), fraction of inspired oxygen (FiO₂), and Respiratory Severity Score (RSS)) were measured at baseline (1 hr pre-procedure), and at 24 hrs & 7 days post. Mean FU was 16.1 mos (SD: 16.6). Paired t-tests & Wilcoxon signed-rank tests were applied.
Results: Twelve infants were included. Mean GA, age & weight at time of procedure were 24.4 wks (SD: 1.5), 25.4 days (SD: 7.6) and 932 gms (SD: 154.4) respectively. The mean PDA diameter was 2.46 mm (SD: 0.47). Comorbidities included muscular ventricular septal defect (1), respiratory distress syndrome (12), necrotizing enterocolitis (1), kidney dysfunction (1), & intraventricular hemorrhage (4). TC PDA occlusion was successful in all with no cases of PLS or residual shunts. Minor adverse events were aortic obstruction (1-mild) and TR (1-mild/moderate); neither required intervention. Two died from unrelated causes – sepsis (1) and short gut syndrome (1) at 13 and 50 days respectively. Mean procedure time was 55.6 min (SD: 10.3), mean fluoroscopy time was 7.2 min (SD: 2.8) and mean contrast volume was 1.8 mL (SD: 1.7). Mean RSS 1 hr pre-procedure was 7.62 (SD: 3.32). MAP showed no significant change at 24 hrs (p = 0.288) but demonstrated a significant reduction by 7 days (p = 0.028). FiO₂ showed a trend towards reduction at 24 hrs (p = 0.087). RSS decreased significantly both at 24 hrs (p = 0.026) and 7 days (p = 0.0058).
Conclusion(s): TC PDA closure in VLBW infants on HFV is safe & effective with minimal complications, short procedural & fluoroscopy times, and minimal contrast. The improvement in RSS at 24 hrs & 7 days suggests that PDA occlusion improves the respiratory status in VLBW infants on HFV. Larger studies are needed to validate these findings and further assess long-term outcomes.
Results table