Back
Background: Despite a continued rise in adolescent obesity and substantial evidence of the safety and efficacy of metabolic and bariatric surgery (MBS), surgical intervention remains underutilized, even in specialized pediatric bariatric surgery centers (PBSCs). Little is known about how MBS is integrated into pediatric residency programs' curricula.
Objective: We aimed to explore pediatric residents’ knowledge of and confidence in counseling adolescents on weight loss surgery. We specifically set out to understand the effect of association with a PBSC on trainees’ perception of and ability to incorporate MBS into their patient counseling. We hypothesized that pediatric residents are not exposed to weight loss surgery in their curricula and lack self-confidence in counseling patients on MBS, regardless of association with a PBSC.
Design/Methods: We designed a brief web-based survey administered to pediatric residents at four institutions, two with an associated PBSC and two without. Data was collected anonymously from January 2022 to July 2022. Relevant data, including residents’ self-reported understanding of indications for adolescent MBS, MBS resources offered at their hospitals, and details of their obesity management curriculum, were analyzed using SAS software, Version 9.4.
Results: Residents at institutions with a PBSC reported higher inclusion of MBS in their didactic curricula than those without a PBSC (50% vs. 12.5%, p< 0.05). However, residents with a PBSC did not report higher confidence in counseling adolescent patients on any modality of obesity management, including surgery. The degree of confidence in counseling patients on any modality of obesity management did not improve with a higher training level. While there was a trend towards identifying the appropriate patient for MBS with a PBSC (85% vs. 62%, p=0.06), this did not translate into higher confidence in correctly referring patients for surgery. By PGY3, both resident cohorts reported greater access to MBS referral resources as compared to trainees in PGY1 and PGY2 (10.5% vs. 29.4% vs. 57.1%, p=0.03).
Conclusion(s): Our study identifies glaringly low self-reported confidence in counseling and referring patients with obesity to any treatment modality in pediatric residents. Although we detected a higher reported exposure to MBS in didactics for residents with an associated PBSC, it did not translate to higher perceived confidence. This calls for the need for more effective resident-directed obesity education to be integrated into curricula as the rates of adolescent obesity continue to rise.
Inclusion of Weight Loss Surgery into Pediatric Residency Curriculum
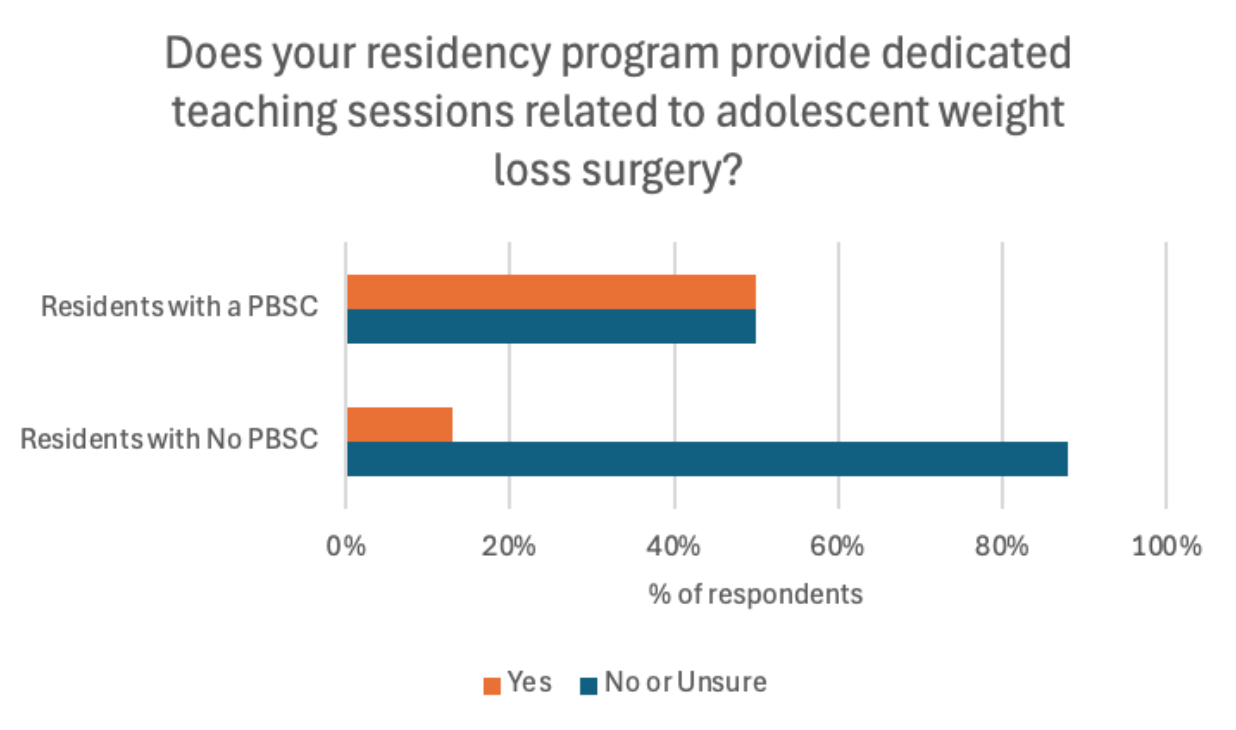 Residents at institutions with Pediatric Bariatric Surgery Centers (PBSCs) report participating in more didactic sessions on weight loss treatment options compared to those at institutions without PBSCs.
Residents at institutions with Pediatric Bariatric Surgery Centers (PBSCs) report participating in more didactic sessions on weight loss treatment options compared to those at institutions without PBSCs.
Residents' Self Reported Confidence in Counseling Patients on Weight Loss Treatment Options
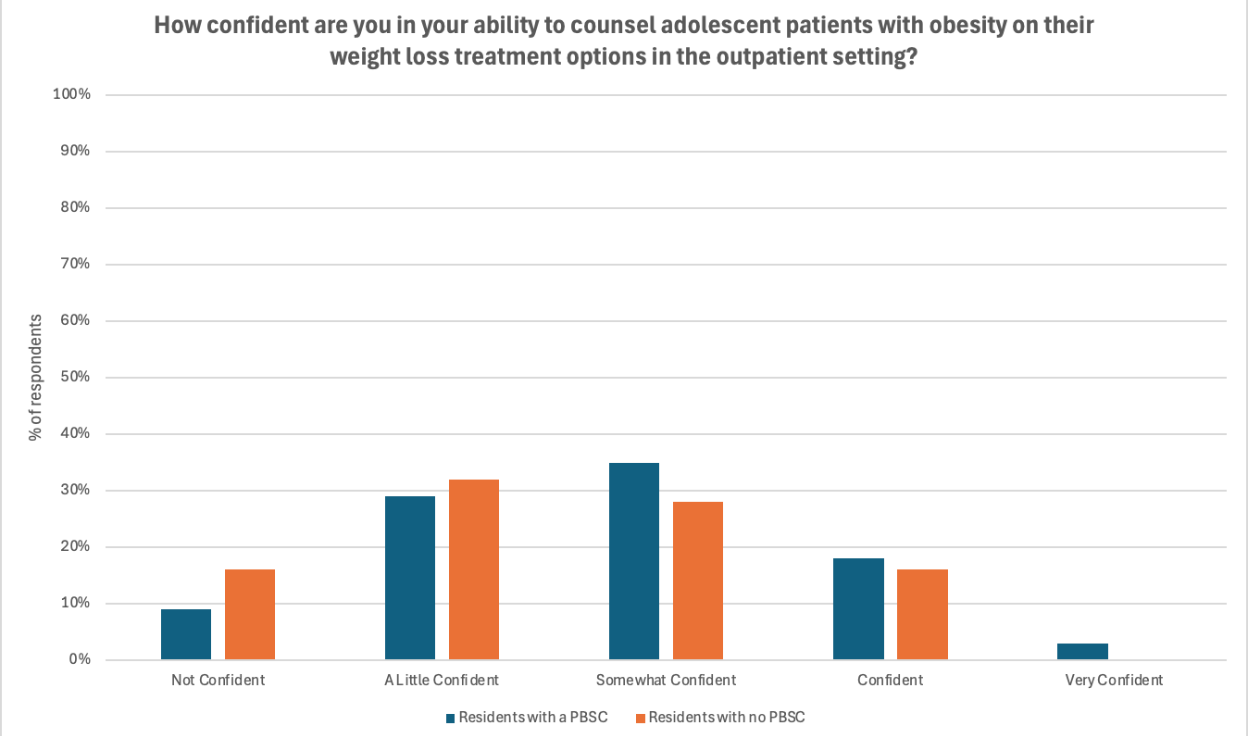 Residents' confidence levels are low, both at institutions with and without PBSCs.
Residents' confidence levels are low, both at institutions with and without PBSCs.
Residents' Perception on Access to Surgical Referral Information
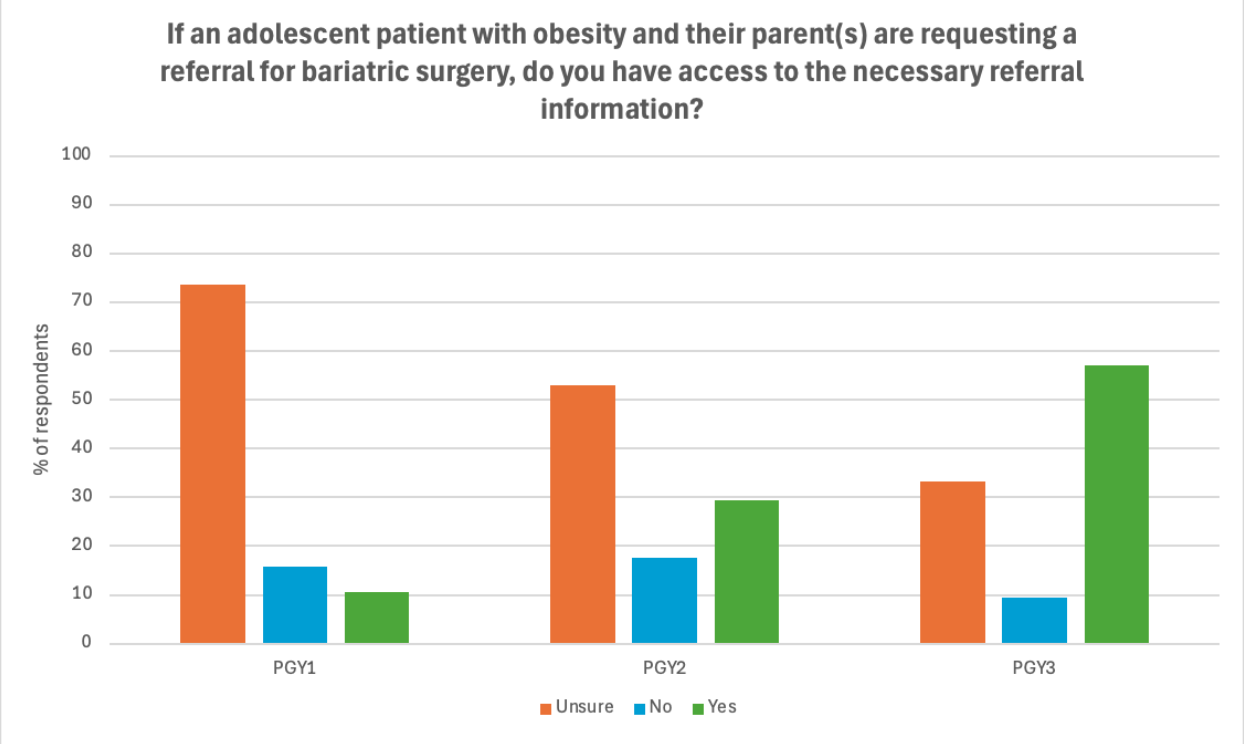 By the end of training, residents at all institutions feel they can find the resources necessary to make an appropriate surgical referral.
By the end of training, residents at all institutions feel they can find the resources necessary to make an appropriate surgical referral.
Medical Education 2: Curricular innovations and assessment 2
Session: Medical Education 2: Curricular innovations and assessment 2
503 - Impact of Pediatric Bariatric Surgery Centers on Pediatric Residents' Knowledge and Confidence in Counseling Adolescents on Metabolic and Bariatric Surgery
Friday, April 25, 2025
5:30pm – 7:45pm HST
Netta Cudkevich, Boston Children's Hospital, Boston, MA, United States; Artur Chernoguz, The Warren Alpert Medical School of Brown University, Milton, MA, United States

Netta Cudkevich, MD (she/her/hers)
Resident
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Despite a continued rise in adolescent obesity and substantial evidence of the safety and efficacy of metabolic and bariatric surgery (MBS), surgical intervention remains underutilized, even in specialized pediatric bariatric surgery centers (PBSCs). Little is known about how MBS is integrated into pediatric residency programs' curricula.
Objective: We aimed to explore pediatric residents’ knowledge of and confidence in counseling adolescents on weight loss surgery. We specifically set out to understand the effect of association with a PBSC on trainees’ perception of and ability to incorporate MBS into their patient counseling. We hypothesized that pediatric residents are not exposed to weight loss surgery in their curricula and lack self-confidence in counseling patients on MBS, regardless of association with a PBSC.
Design/Methods: We designed a brief web-based survey administered to pediatric residents at four institutions, two with an associated PBSC and two without. Data was collected anonymously from January 2022 to July 2022. Relevant data, including residents’ self-reported understanding of indications for adolescent MBS, MBS resources offered at their hospitals, and details of their obesity management curriculum, were analyzed using SAS software, Version 9.4.
Results: Residents at institutions with a PBSC reported higher inclusion of MBS in their didactic curricula than those without a PBSC (50% vs. 12.5%, p< 0.05). However, residents with a PBSC did not report higher confidence in counseling adolescent patients on any modality of obesity management, including surgery. The degree of confidence in counseling patients on any modality of obesity management did not improve with a higher training level. While there was a trend towards identifying the appropriate patient for MBS with a PBSC (85% vs. 62%, p=0.06), this did not translate into higher confidence in correctly referring patients for surgery. By PGY3, both resident cohorts reported greater access to MBS referral resources as compared to trainees in PGY1 and PGY2 (10.5% vs. 29.4% vs. 57.1%, p=0.03).
Conclusion(s): Our study identifies glaringly low self-reported confidence in counseling and referring patients with obesity to any treatment modality in pediatric residents. Although we detected a higher reported exposure to MBS in didactics for residents with an associated PBSC, it did not translate to higher perceived confidence. This calls for the need for more effective resident-directed obesity education to be integrated into curricula as the rates of adolescent obesity continue to rise.
Inclusion of Weight Loss Surgery into Pediatric Residency Curriculum
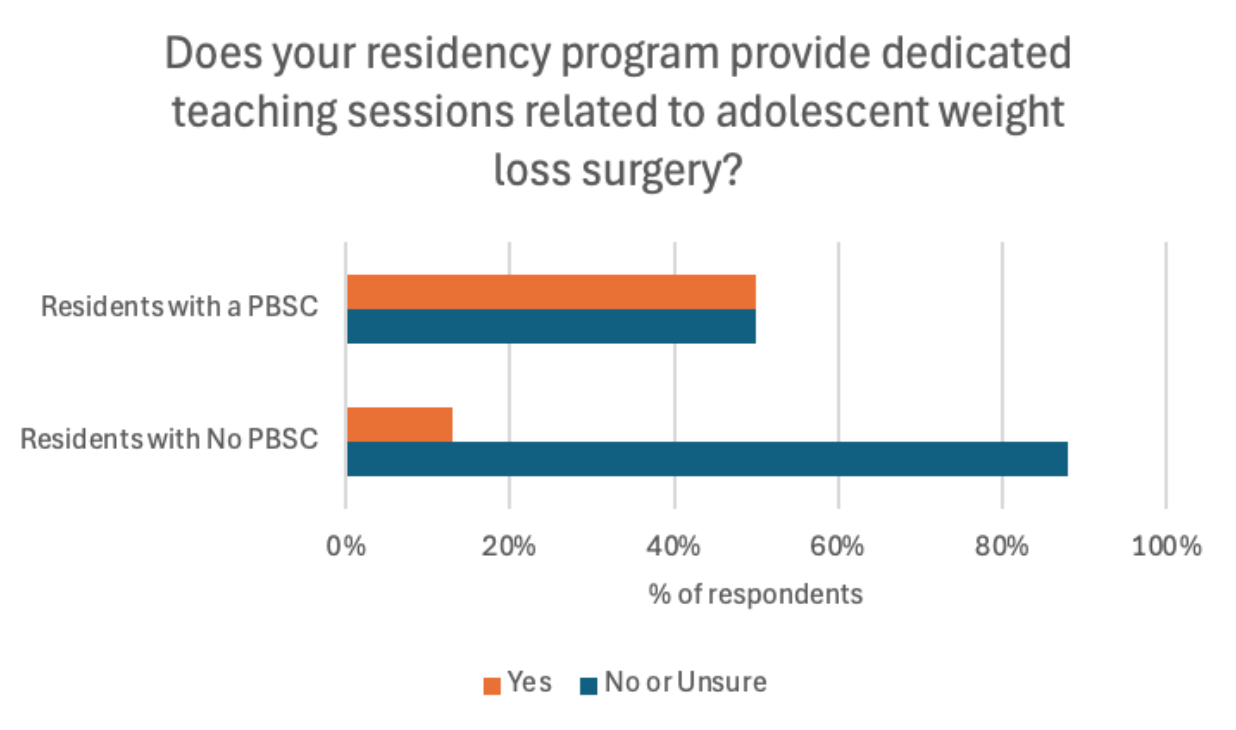 Residents at institutions with Pediatric Bariatric Surgery Centers (PBSCs) report participating in more didactic sessions on weight loss treatment options compared to those at institutions without PBSCs.
Residents at institutions with Pediatric Bariatric Surgery Centers (PBSCs) report participating in more didactic sessions on weight loss treatment options compared to those at institutions without PBSCs.Residents' Self Reported Confidence in Counseling Patients on Weight Loss Treatment Options
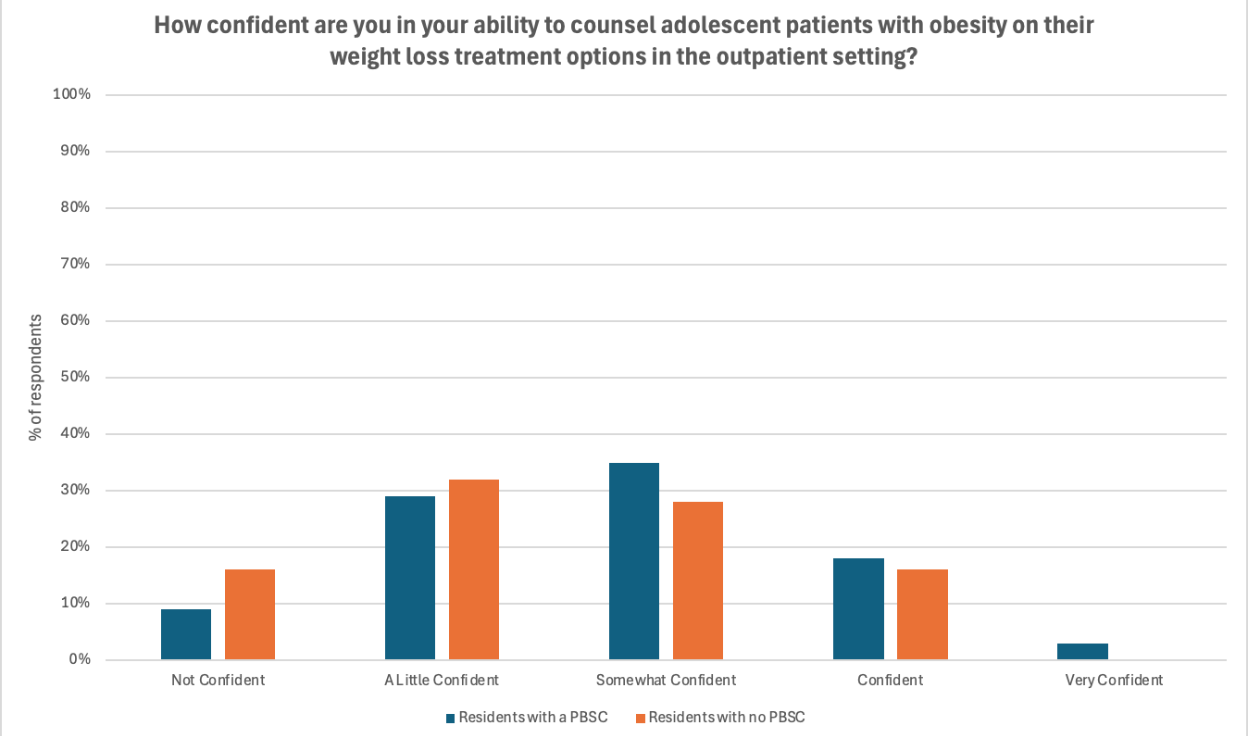 Residents' confidence levels are low, both at institutions with and without PBSCs.
Residents' confidence levels are low, both at institutions with and without PBSCs. Residents' Perception on Access to Surgical Referral Information
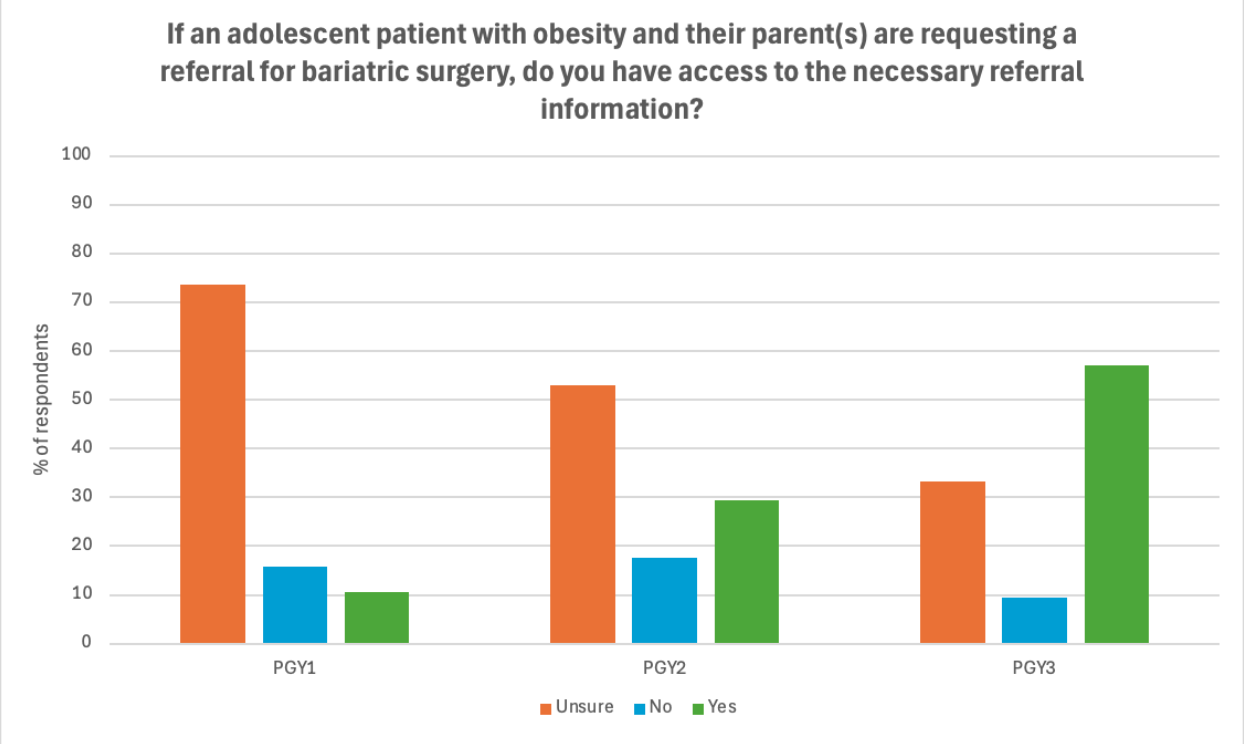 By the end of training, residents at all institutions feel they can find the resources necessary to make an appropriate surgical referral.
By the end of training, residents at all institutions feel they can find the resources necessary to make an appropriate surgical referral. 
