Global Neonatal & Children's Health 2
Session: Global Neonatal & Children's Health 2
743 - Multi-Center, Multinational Validation of the Pediatric Early Warning Score for Resource-Limited Settings (PEWS-RL)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 743.5715
Marisa Cristin Woo, University of Hawaii, John A. Burns School of Medicine, San Jose, CA, United States; Adnan T. Bhutta, Indiana University School of Medicine, Indianapolis, IN, United States; Adrian Holloway, University of Maryland School of Medicine, Baltimore, MD, United States; Asya Agulnik, St. Jude Children's Research Hospital, Memphis, TN, United States; Teresa Kortz, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Marisa Cristin Woo, MS (she/her/hers)
Medical student
University of Hawaii, John A. Burns School of Medicine
San Jose, California, United States
Presenting Author(s)
Background: Pediatric Early Warning Systems (PEWS) are evidence-based tools that support early detection of clinical deterioration in hospitalized children. Resource-limited settings (RLS) have high pediatric hospital mortality and face unique challenges managing clinical deterioration. The PEWS for Resource-Limited Settings (PEWS-RL) is a previously adapted PEWS provisionally validated in a large tertiary hospital in Rwanda. It has not, however, been evaluated in other RLS.
Objective: To test the discriminative ability of PEWS-RL to identify clinical deterioration events (CDE) in the day following hospital presentation due to an acute illness or injury.
Design/Methods: We conducted a secondary analysis of the Global Pediatric Acute Critical Illness Point Prevalence Study (Global PARITY), a multinational prospective point-prevalence study. Global PARITY measured the burden of acute critical illness in RLS in children 28 days-14 years old and included 7,538 children from 46 sites across 19 countries from July 2021-July 2022. Of these, we included subjects admitted to the hospital or who died in the emergency department and excluded those transferred to another facility, discharged, absconded, or directly admitted to the intensive care or high dependency unit. We calculated PEWS-RL on hospital presentation using 6 equally weighted variables: heart rate, respiratory rate, temperature, systolic blood pressure, supplemental oxygen use, presence of respiratory distress, and validated mental status scales. We defined a CDE as death, use of cardiopulmonary resuscitation, noninvasive respiratory support, mechanical ventilation, vasoactives, or ICU transfer within the first hospital day. We calculated the area under the receiver operating characteristic (AUROC), sensitivity, and specificity for PEWS-RL to predict CDE.
Results: Among 2,557 patients who met inclusion criteria, 1,264 (49.4%) had no missing components of PEWS-RL based on documented vital signs and were included in this analysis. Of these, median age was 3 years (interquartile range 1-7 years), and 44.2% were female. Seventy-three (5.8%) patients experienced at least one CDE, and 12 died on the day of hospital presentation. The PEWS-RL score at the time of presentation was correlated with subsequent CDE (Figure 1) with an AUROC of 0.8363. A PEWS-RL score ≥3 had a sensitivity of 60.3% and specificity of 88.6% to predict CDE.
Conclusion(s): This multi-center, multinational study further validates PEWS-RL to identify children at high-risk of a CDE in RLS; however, accuracy of the tool depends on appropriate documentation of complete vital signs required for calculation.
Figure 1: Receiver operating characteristic (ROC) curve
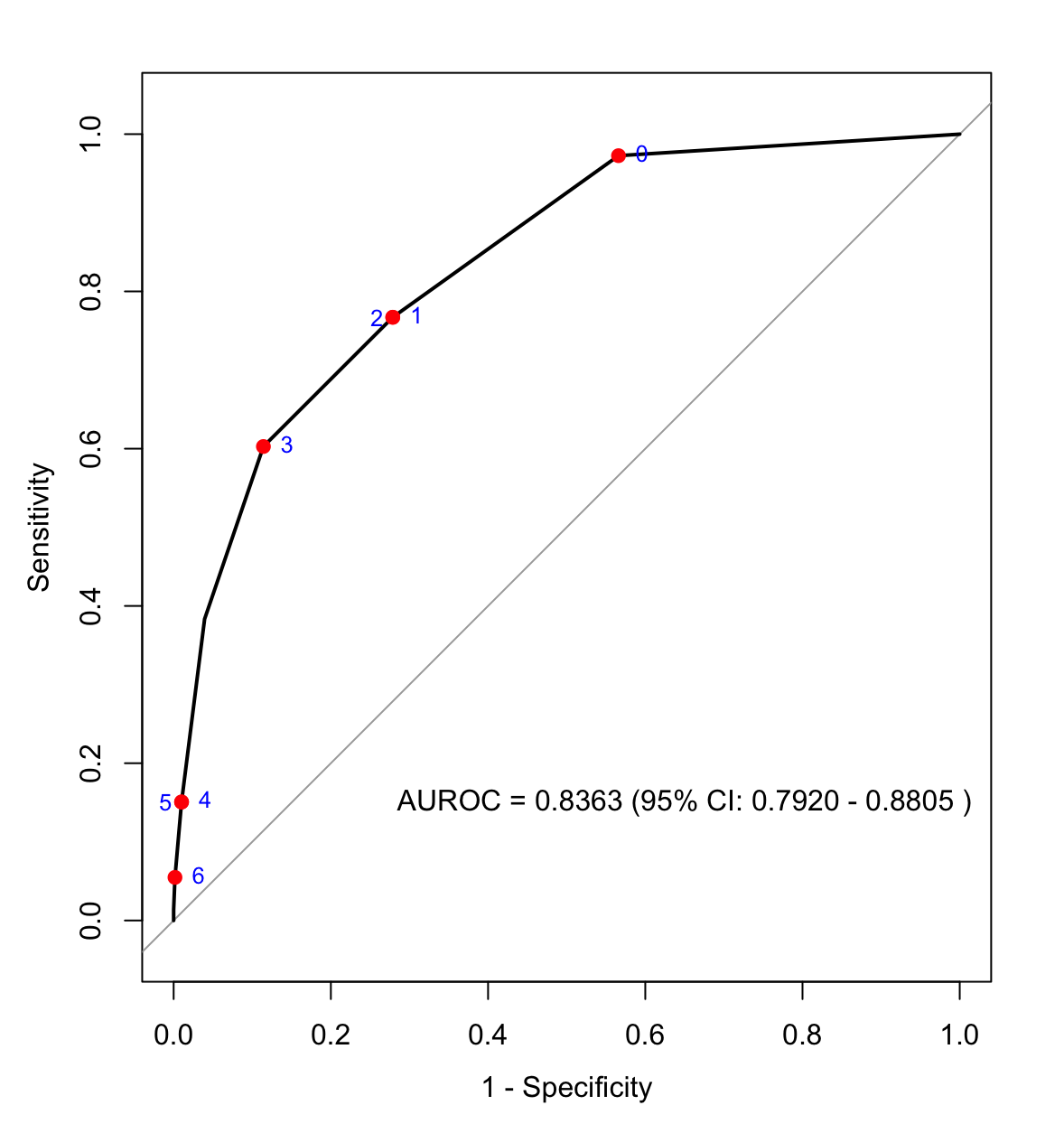 Figure 1: The receiver operating characteristic (ROC) curve shows the discriminative ability of the Pediatric Early Warning Score for Resource-Limited Settings (PEWS-RL) to identify clinical deterioration events (CDE) in the day following hospital presentation due to an acute illness or injury. The area under the ROC (AUROC) was 0.8363 [95% confidence interval, 0.7920-0.8805]. A PEWS-RL score ≥3 had a sensitivity of 60.3% and specificity of 88.6% to predict CDE.
Figure 1: The receiver operating characteristic (ROC) curve shows the discriminative ability of the Pediatric Early Warning Score for Resource-Limited Settings (PEWS-RL) to identify clinical deterioration events (CDE) in the day following hospital presentation due to an acute illness or injury. The area under the ROC (AUROC) was 0.8363 [95% confidence interval, 0.7920-0.8805]. A PEWS-RL score ≥3 had a sensitivity of 60.3% and specificity of 88.6% to predict CDE.
