Allergy, Immunology, and Rheumatology 2
Session: Allergy, Immunology, and Rheumatology 2
651 - Maternal Penicillin Allergy and Congenital Syphilis
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 651.6002
Laura Ann Wang, University of Colorado School of Medicine, Aurora, CO, United States; Kathryn McKenney, University of Colorado School of Medicine, Aurora, CO, United States; Sean T. O'Leary, University of Colorado School of Medicine, Denver, CO, United States

Laura Ann Wang, MD, MPH (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Syphilis cases have increased sharply across the US over the last decade. Syphilis can be directly transmitted from mothers to infants during pregnancy and can result in congenital syphilis.
The only effective treatment for syphilis infection during pregnancy is penicillin G. However, approximately 10% of the population reports a history of penicillin allergy. As such, a maternal history of penicillin allergy may be a potential factor contributing to inadequate treatment of syphilis in pregnancy.
Objective: To characterize a cohort of mothers with a penicillin allergy label and syphilis infection during pregnancy and the clinical outcomes of their infants.
Design/Methods: We performed a retrospective cohort study of infants born to women with a reported penicillin allergy and diagnosis of syphilis during pregnancy who received care at a single center between 2020 and 2024. We identified infants using an ICD-10 code correlating with exposure to syphilis during pregnancy. Infants identified electronically were confirmed through individual chart review. We included those with a maternal penicillin allergy label and excluded any whose mothers did not have documentation of positive syphilis test result at diagnosis.
Results: We identified 78 infants with exposure to syphilis during pregnancy and 12 whose mothers had a penicillin allergy label. There were 8 infants whose mothers were diagnosed with syphilis prior to delivery who had a penicillin allergy label; all initiated treatment with penicillin prior to delivery. Five of these mothers underwent and passed penicillin allergy evaluation during pregnancy, 2 underwent direct penicillin desensitization, and 1 was administered the first dose of penicillin in the emergency room without testing or desensitization; 6/8 completed treatment prior to delivery. Mothers of 4 infants were not diagnosed until their delivery hospitalization. The majority of infants fell into Red Book classification of “possible congenital syphilis” (50%) or “confirmed or highly probable congenital syphilis” (16.7%).
Conclusion(s): Mothers with a maternal penicillin allergy and syphilis diagnosis in pregnancy in this cohort mostly received appropriate management and treatment with penicillin. Failure to complete treatment and diagnosis of syphilis during the delivery encounter appear to be major contributors to infant syphilis diagnosis. Further research in larger populations is needed to determine the impact of a penicillin allergy label on infant outcomes and how best to promote maternal syphilis diagnosis and treatment during pregnancy.
Table 1
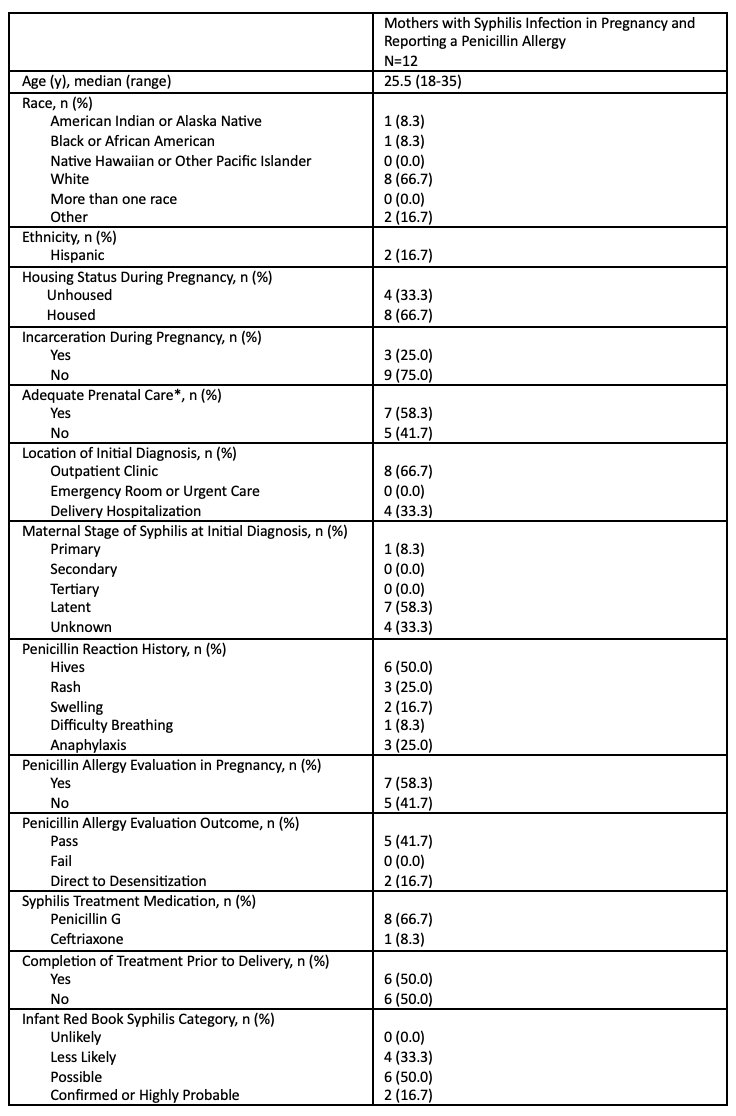 Characteristics and management of mothers reporting a penicillin allergy during pregnancy and clinical outcomes of their infants
Characteristics and management of mothers reporting a penicillin allergy during pregnancy and clinical outcomes of their infants
