Cardiology 3
Session: Cardiology 3
166 - Natural History of Troponin I elevation in pediatric emergency room patients
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 166.5989
Jenil M. Rana, University of North Texas Health Science Center, North Richland Hills, TX, United States; Samuel Selby, UNTHSC TCOM, Fort Worth, TX, United States; Robert Loar, Cook Children's Medical Center, Fort Worth, TX, United States

Jenil M. Rana, OMS-II (he/him/his)
Medical Student
University of North Texas Health Science Center
North Richland Hills, Texas, United States
Presenting Author(s)
Background: The use of troponin I (TnI) is common in pediatric emergency rooms as a screening for cardiac injury/ischemia.
Objective: We hypothesize that in pediatric patients presenting to a local ER, the natural history of trivially elevated troponin is normal without cardiac sequelae as evident by subsequent cardiac testing. Additionally, we hypothesized there exists a cut-off troponin value with good sensitivity and specificity for associated abnormal cardiac testing.
Design/Methods: We conducted a single-center retrospective study of patients who were presented to Cook Children’s ER 2022-2023 with an abnormal troponin level. Patients without elevated troponin or follow-up cardiac testing were excluded. Each patient’s hospital course was captured and collected. We compared patients with normal (normal EKG + ECHO) versus abnormal (abnormal EKG + ECHO) cardiac findings using chi-square and independent t-tests. Receiver operating curve analysis to determine discriminatory ability of troponin. Sensitivity and specificity were determined using Youden’s J statistic. Sub-groups were compared by independent t-test and Chi-square, where appropriate, and p < 0.05 was considered significant.
Results: There were 465 patients who met inclusion criteria for analysis, of which 38 had abnormal cardiac testing and 427 had normal testing. There were no differences in age, sex, prior cardiac disease, or size (Table). Patients with abnormal cardiac testing had significantly higher troponin (5.4 ± 11.0 vs. 0.47 ± 2.0, p < 0.001) and BNP levels (356 ± 1189 vs 2113 ± 4003, p < 0.001). Abnormal cardiac testing group also experienced significantly higher rates of hospital admission, ICU admission, inotropic support, and ECMO support. ROC analysis demonstrated good discriminatory ability for troponin to detect patients with subsequent abnormal cardiac testing (area under curve = 0.84, p < 0.001). Point of best sensitivity and specificity was a troponin value of 0.2 – sensitivity 76.3% and specificity 81%. A troponin < 0.2 yielded a negative predictive value of 98% for abnormal cardiac testing. Patients with troponin < 0.2 experienced hospital admission 68.1% of the time, ICU admission 29.4%, inotrope use 14.8%, ECMO use 1.1%.
Conclusion(s): Troponin levels at ER presentation has good discriminatory ability for associated abnormal cardiac testing. Low troponin levels ( < 0.2) have high negative predictive value, though many pediatric patients with TnI < 0.2 still experienced a hospital admission. This data could guide ER triage and resource use.
Patient demographics and Clinical Characteristics.
.png) Comparison of Normal testing group to Abnormal testing group. P-value < 0.05 considered statistically significant, marked in bold font.
Comparison of Normal testing group to Abnormal testing group. P-value < 0.05 considered statistically significant, marked in bold font. Receiver Operating Characteristic Curve.
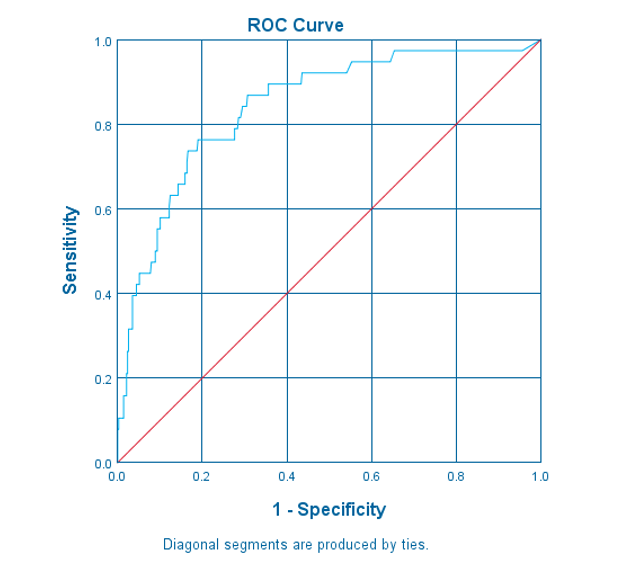 Receiver operating characteristic analysis of troponin levels at ER presentation for associated abnormal cardiac testing.
Receiver operating characteristic analysis of troponin levels at ER presentation for associated abnormal cardiac testing.
