General Pediatrics 2
Session: General Pediatrics 2
717 - Investigating the relationship between ACE screening and referrals among pediatric patients in primary care
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 717.5739
India Gill, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Andrew V. Nguyen, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Morgan Ye, University of California, San Francisco, School of Medicine, Dublin, CA, United States; Celia Draycott, ACEs-LA, Los Angeles County Health Services, Brooklyn, NY, United States; Nina N. Thompson, Olive View-UCLA Education and Research Institute, San Francisco, CA, United States; Amy Shekarchi, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Danielle Hessler Jones, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Dayna Long, UCSF Benioff Children's Hospital Oakland, Oaklnad, CA, United States; Matthew S. Pantell, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Neeta Thakur, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Edward Machtinger, University of California, San Francisco, San Francisco, CA, United States; Shannon M.. Thyne, David Geffen School of Medicine at UCLA, SYLMAR, CA, United States

India Gill, MPH, PhD (she/her/hers)
Postdoctoral Fellow
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Adverse childhood experiences (ACEs) are linked to long-term health consequences, including chronic diseases, mental health disorders, and social challenges. ACE screening in primary care offers an opportunity for early intervention. ACE screening is increasingly being implemented in pediatric primary care, however the impact of screening on referrals remains underexplored.
Objective: This study assessed the relationship between ACE screening of children and the likelihood of receiving medical, mental health, or social care referrals in a large safety-net system.
Design/Methods: We conducted a retrospective chart review of Los Angeles County Department of Health Services pediatric patients (0-17 years) screened for ACEs in 10 clinics from 11/2021 - 5/2023. The primary outcome was whether any referrals were submitted within six months of screening between 11/2021 - 11/2023. We examined two referral platforms: One Degree, a referral system for social care community resources and eConsult, an electronic health record-embedded platform for medical specialty referrals. Propensity score matching controlled for confounders, matching screened and non-screened patients. Logistic regression analyses were performed to compare likelihood for eConsult and One Degree referrals among: (1) those screened and not screened and (2) those with 0 ACEs, ≥1 ACEs, and not screened.
Results: Among 10,422 children, the average age was 8.7 years, 51.3% were male, 71.5% were Latino, 15.9% had an eConsult and 0.7% had a One Degree referral. Screened children were more likely to have an eConsult referral (odds ratio (OR): 1.30, 95% CI: 1.16, 1.45), including those with 0 ACEs (OR: 1.30, 95% CI: 1.15, 1.47) and those with ≥1 ACEs (OR: 1.64, 95% CI: 1.35, 1.98) compared to non-screened children. Black and Latino screened patients were more likely to receive eConsult referrals (Table 1). All screened children had higher odds of medical and mental health eConsult referrals (Table 2). ACE screening was also associated with an increased odds of a One Degree referral (OR: 4.42, 95% CI: 2.49, 7.83), including both 0 ACEs (OR: 3.37, 95% CI: 1.86, 6.40) and ≥1 ACEs (OR: 7.00, 95% CI: 3.38, 14.66) score groups compared to non-screened children.
Conclusion(s): ACE screening significantly increased the likelihood of eConsult and One Degree referrals. Findings support the integration of ACE screening in safety-net primary care to better address medical, mental health, and social care referrals. Expanding ACE screening in primary care may enhance early intervention efforts and improve health and social outcomes for children in underserved communities.
Curriculum Vitae_India Gill_2024.pdf
Table 2. Odds Ratios of eConsult and One Degree Referrals within Six Months of ACE Screening (n=10422)
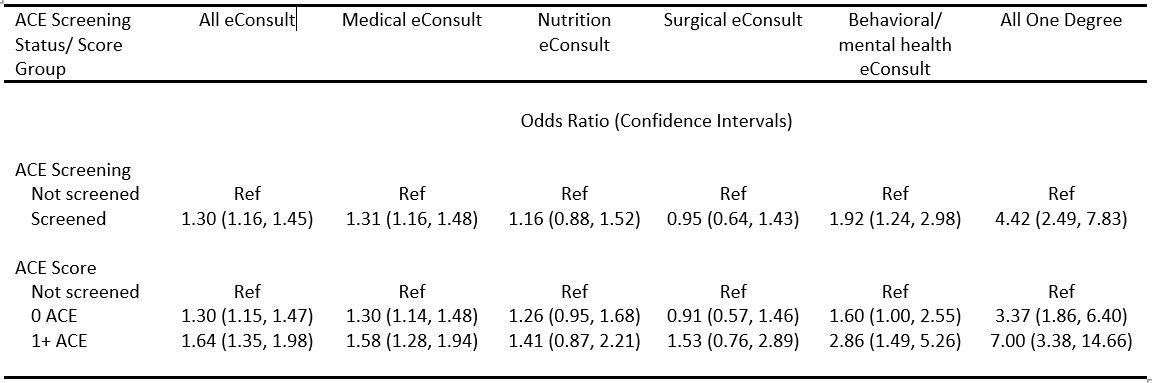 Reference group is non-screened pediatric patients. Patients were propensity score matched on age, gender, clinic, insurance, appointment type, number of primary care visits, and primary care visit date quartile. Outcome models were further adjusted for covariates with standardized mean differences exceeding 0.2.
Reference group is non-screened pediatric patients. Patients were propensity score matched on age, gender, clinic, insurance, appointment type, number of primary care visits, and primary care visit date quartile. Outcome models were further adjusted for covariates with standardized mean differences exceeding 0.2.
