Quality Improvement/Patient Safety 1
Session: Quality Improvement/Patient Safety 1
013 - Multidisciplinary lupus clinic for childhood onset SLE.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 13.5741
Ankana Daga, Boston Children's Hospital, Boston, MA, United States; Esra Meidan, Boston Children's Hospital, BOSTON, MA, United States; Maria G. Biancarelli, Boston Children's Hospital, Brookline, MA, United States; Amy Mcdonough, Boston Children’s Hospital, Braintree, MA, United States; Caitlyn Dorsey, Boston Children's Hospital, Boston, MA, United States; Anthony Dekermanji, Boston Children's Hospital, Boston, MA, United States; Benjamin Ethier, Boston Children's Hospital, San Diego, CA, United States; Brittany Esty, Boston Children's Hospital, Boston, MA, United States; Melissa Hazen, Boston Children's Hospital, Boston, MA, United States

Melissa M. Hazen, MD (she/her/hers)
Assistant Professor of Pediatrics
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Childhood-onset systemic lupus erythematosus (cSLE) is a complex autoimmune disorder marked by significant disease severity and multisystem involvement. The variability in care often leads to lapses in essential screenings and treatment-related toxicity. A multidisciplinary management approach is crucial for effective cSLE care; however, such clinics are scarce.
Objective: This study aims to establish a multidisciplinary lupus clinic at our center to standardize management through a "lupus clinic form" (Fig 1) emphasizing appropriate screening and monitoring for medication toxicity. Our targets include increasing timely pulmonary function test (PFT) screening to 50%, echocardiogram screening to over 30%, and reducing the percentage of patients on high-dose steroids from 63% to below 30% by April 2024.
Design/Methods: A self-identified multidisciplinary team was formed to develop the lupus clinic and tackle existing care challenges. We conducted direct observations and a root cause analysis using a fishbone diagram to assess current practices. Based on these findings, a lupus clinic form was created, undergoing multiple Plan-Do-Study-Act (PDSA) cycles from December 2022 to April 2024, focusing on education, dissemination, and workflow improvements.
Results: The pediatric lupus clinic successfully launched with a team comprising a pediatric rheumatologist, nephrologist, nurse, social worker, and research coordinator. We served 20 complex cSLE patients, with a demographic profile of 50% non-English speaking, 45% Hispanic, 20% Black, and an average age of 18 years; 90% were female and 75% came from lower socioeconomic backgrounds reliant on public insurance. The clinic demonstrated high follow-up rates, with only one patient requiring subsequent emergency room visits. Notably, 32% of patients in the lupus clinic underwent PFTs, compared to less than 27 outside the clinic (Fig 2). Additionally, 43% of patients in the lupus clinic received echocardiograms according to the recommended schedule versus 28% seen in non-lupus clinic settings, and the percentage of patients on high-dose steroids was lower in the lupus clinic cohort (Fig 3).
Conclusion(s): Our multidisciplinary lupus clinic offers high-quality, coordinated care through shared clinical appointments and collaborative decision-making for this severe disease. The promising outcomes suggest improved follow-up care and treatment adherence, while providing a framework for rapid testing of interventions to optimize health for children with cSLE.
Lupus Clinic Form
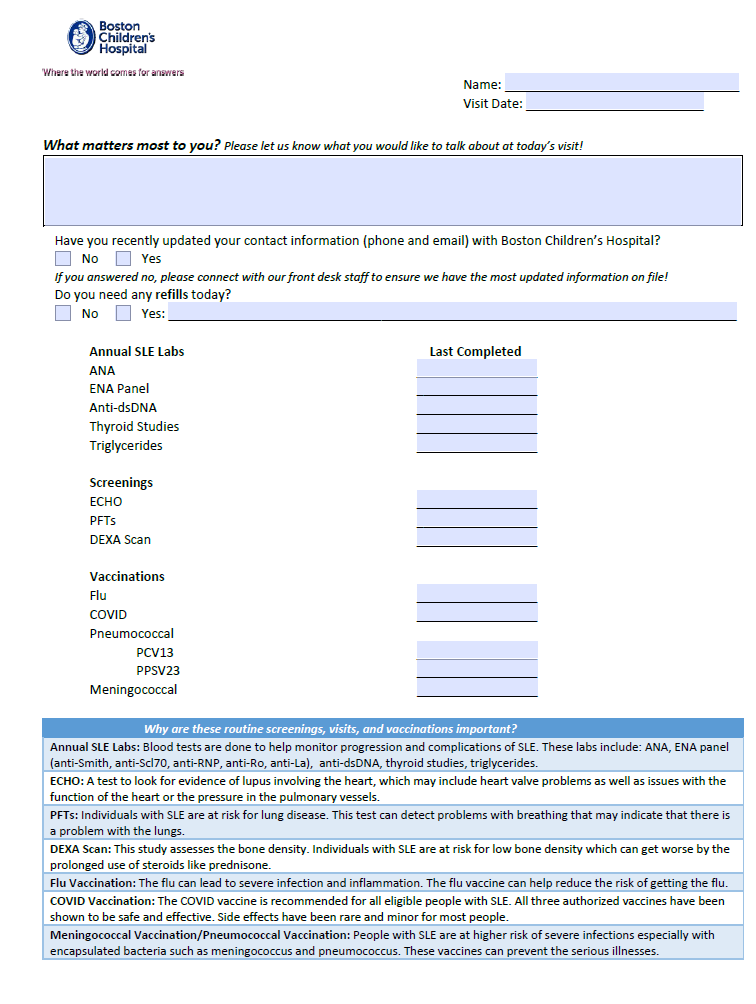 Fig 1
Fig 1PFTs in lupus clinic vs non lupus clinic
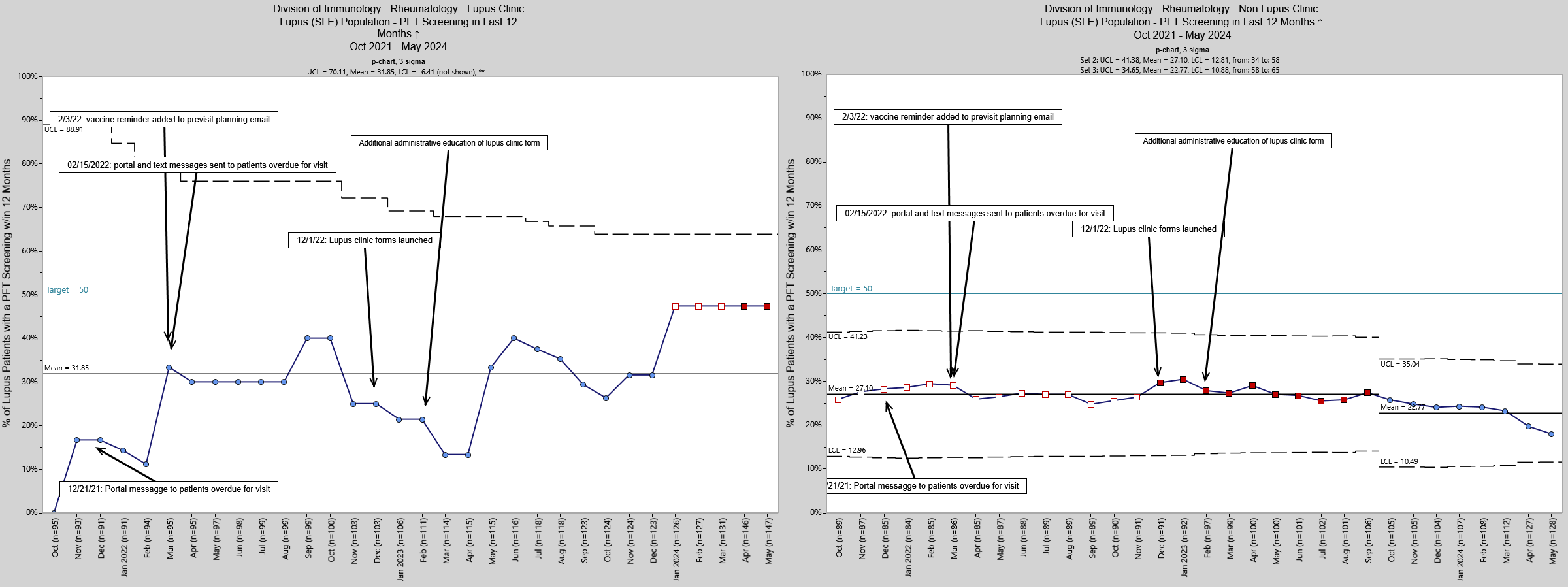 Fig 2
Fig 2Steroid use in Lupus Clinic vs non lupus clinic
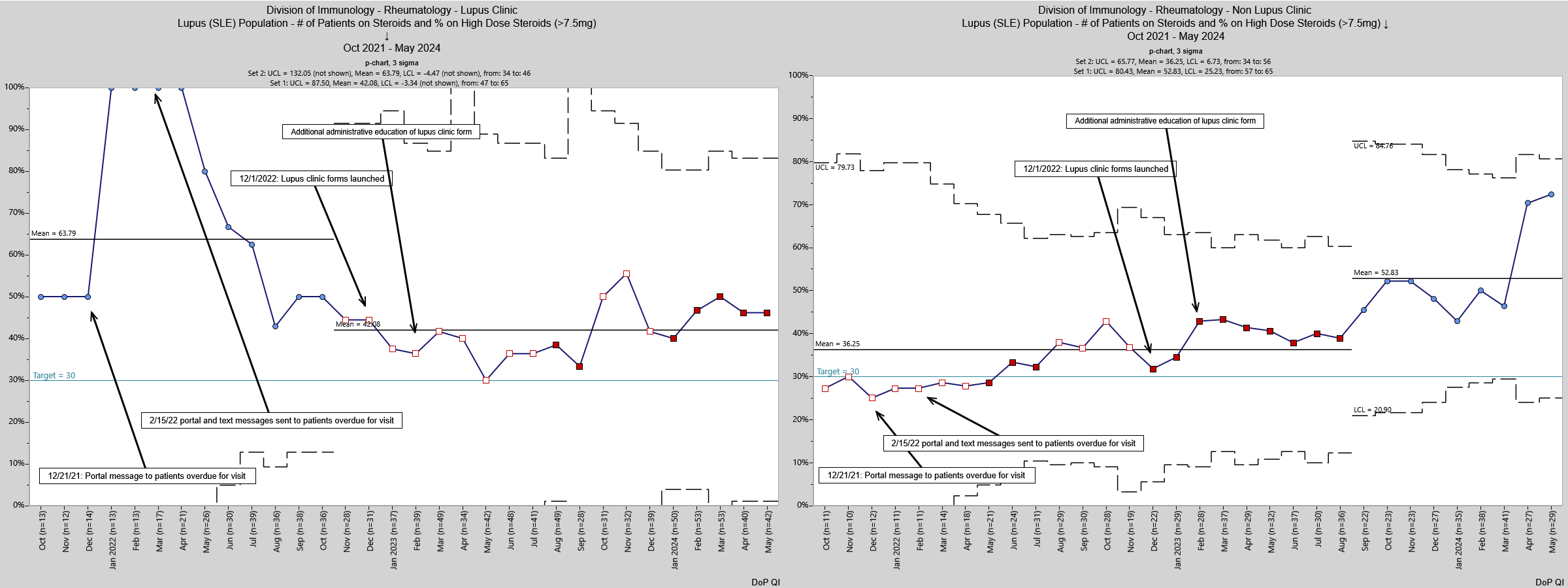 Fig 3
Fig 3

