Cardiology 1
Session: Cardiology 1
137 - Impact of Obstructive Sleep Apnea on Inpatient Hospitalization Outcomes in Children with Congenital Heart Disease Admitted for Acute Lower Respiratory Tract Infections
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 137.5560
Harshitha Dhanpalreddy, Charleston Area Medical Center, Charleston, WV, United States; Aravind Thavamani, UH Rainbow Babies & Children's Hospital, Cleveland, OH, United States; Jasmine Khatana, UH Cleveland Medical Center, Cleveland, OH, United States; Krishna Kishore Umapathi, West Virginia University- Charleston Division, Charleston, WV, United States
- HD
Harshitha Dhanpalreddy, MBBS MSc (she/her/hers)
Resident Physician
Charleston Area Medical Center
Charleston, West Virginia, United States
Presenting Author(s)
Background: Children with congenital heart disease (CHD) are at higher risk for lower respiratory tract infections (LRTI). OSA has an adverse effect on cardiovascular health. Studies have also shown a bidirectional relationship between LRTI and OSA. However, there is a paucity of large-scale data evaluating the impact of OSA on outcomes in hospitalizations for LRTI among children with congenital heart disease (CHD).
Objective: To evaluate the impact of OSA among children in the United States with CHD admitted for LRTI using large scale data. We hypothesize that the presence of OSA adversely impacts hospital outcomes among children with underlying CHD hospitalized with LRTI.
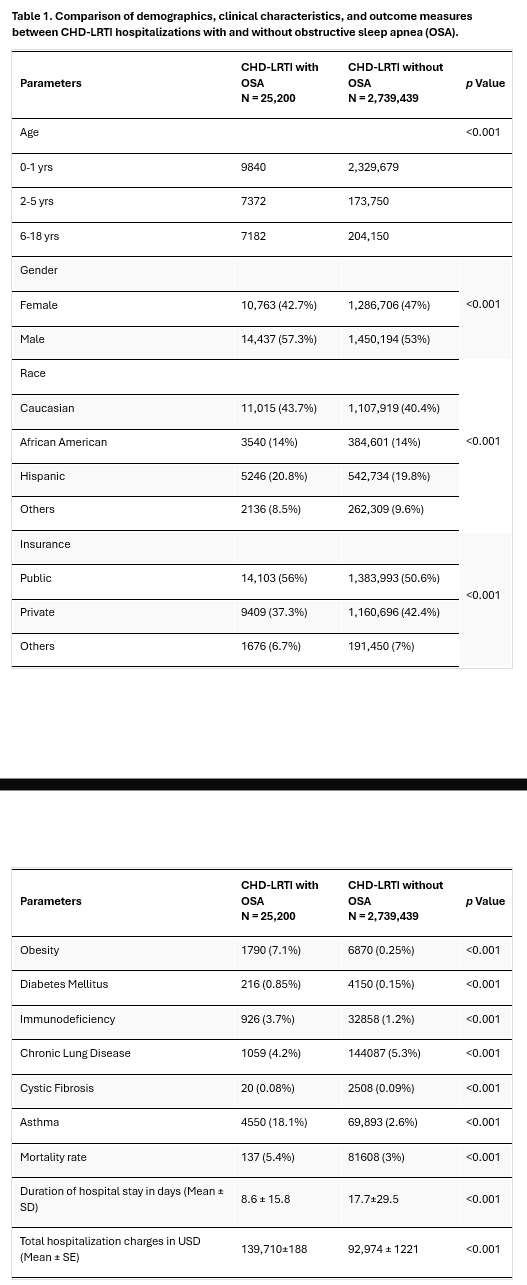
Design/Methods: We analyzed the National Inpatient Sample and Kids Inpatient Database to include all pediatric CHD hospitalizations with a primary diagnosis of LRTI between 2003–2019. Using ICD codes, the CHD-LRTI cohort was divided into two groups: those with and those without a concomitant diagnosis of OSA. The primary outcome was in-hospital mortality. The secondary outcomes were the lengths of each hospital stay and total hospitalization charges.
Results: We analyzed 2,763,665 hospitalizations during the 17-year study period. The overall prevalence rate of OSA was 0.9%. CHD patients with LRTI and OSA were significantly older and were more often male, p < 0.001. The overall mortality rate in the OSA group was 5.4% vs 3% in the non OSA group, and multivariate regression analysis after adjusting for comorbidities like obesity, asthma, cystic fibrosis, immunodeficiency, diabetes mellitus, and chronic lung disease still showed that OSA was associated with 2.3 times higher odds of in-hospital mortality (95% CI: 1.4 to 5.6, p < 0.001). Linear regression analyses demonstrated that OSA independently contributed an additional 5.8 days to the hospital stay length (95% CI: 3.9 to 8.6, p < 0.001) and an extra 30,479 USD (95% CI: 29,110 to 32,848, p < 0.001) in hospitalization charges.
Conclusion(s): Among children with CHD admitted for LRTI, OSA is associated with poor hospital outcomes such as increased mortality risk and increased healthcare utilization.
Table 1. Comparison of demographics, clinical characteristics, and outcome measures between CHD-LRTI hospitalizations with and without obstructive sleep apnea (OSA)