Quality Improvement/Patient Safety 3
Session: Quality Improvement/Patient Safety 3
034 - Impacting Continuity of Care through Systematic Patient Empanelment
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 34.5524
Michael Garbe, Oklahoma Childrens Hospital at OU Health, Oklahoma City, OK, United States; Paul M. Darden, University of Oklahoma College of Medicine, Oklahoma City, OK, United States; Sowmya Patil, University of Arkansas for Medical Sciences College of Medicine, LR, AR, United States; Christopher E. Smith, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Kelly A. Curran, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States; Ryan M. Breaud, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States
- MG
Michael Garbe, MPH
Research Assistant and PhD Candidate
Oklahoma Childrens Hospital at OU Health
Oklahoma City, Oklahoma, United States
Presenting Author(s)
Background: Continuity of patient care, ensuring patients see the same provider over time, is important and associated with improved patient satisfaction, patient outcomes, provider satisfaction and lower costs of care. Patient empanelment, the act of assigning patients to clinicians, is an administrative action that is necessary for improving continuity of patient care.
Objective: Our objective was to test whether systematic empanelment improves continuity of patient care.
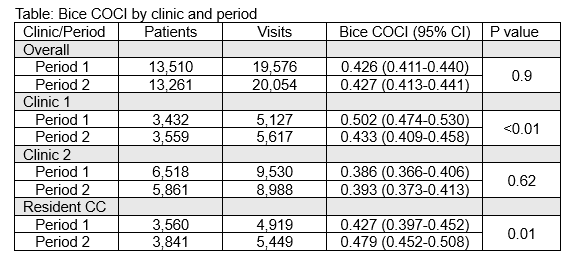
Design/Methods: In three clinics, two attending/APRN only (Clinic 1 and Clinic 2) and one pediatric resident continuity clinic (Resident CC) with centralized scheduling, patients less than 21 years old were empaneled to clinicians based on their visit history (engagement). Empanelment was, first, to a specific clinic and then to a specific clinician. Empanelment procedures followed the 4-cut method, a series of steps aimed at assigning patient to clinicians they have seen most frequently. The outcome was the Bice Continuity of Care Index (COCI) measured by period, 5 months before and 5 months after empanelment. COCI was measured by patient within clinic and period. For a patient to contribute to COCI a patient must have 2 visits within the period. Period comparisons by clinic were made using t-tests.
Results: Overall, 26,771 patients and 39,630 visits in 3 clinics were examined. Baseline continuity measurements were significantly different between the two attending/APRN clinics (0.5, 95% CI: 0.47-0.53 vs. 0.39, 95% CI: 0.37-0.41). Multivariable analysis demonstrated the association between period and Bice COCI significantly differs between clinics, resulting in interaction. Thusly, clinic-specific associations are reported. The results by clinic showed clinic 1 with significantly higher Bice COCI in period 1 decreasing in period 2 (p <.01). Resident CC Bice COCI increased significantly between periods 1 and 2 (p=.01). There was no significant difference in Bice COCI between periods for Clinic 2 (p=.62).
Conclusion(s): Empanelment is necessary for supporting and improving continuity of patient care. Systematic methods of empanelment should be studied to achieve the greatest possible impact on continuity of patient care. Clinic and leadership engagement is critical for improvement even with centralized scheduling. The pediatric resident continuity clinic embraced empanelment and leadership worked with clinicians, nurses and scheduling to support and extend continuity of care. We need to further explore clinic factors associated with these disparate results.
BICE COCI by Clinic and Period